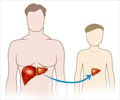
To reduce operating room revisits it is advisable not to match an obese liver transplant recipient with an alcoholic donor.
- There is a higher incidence of return to the operating room in obese patients, with an increased risk of coagulopathy, who receive a liver from an alcoholic patient
- Understanding this can help clinicians to plan better for their patients during and after surgery
The R-OR rate for liver transplant patients with a body mass index (BMI) greater than 30 and who were matched with livers from donors with a history of heavy alcohol use was 80%. The trio of obesity, excessive alcohol consumption and coagulopathy- a diminished capacity to produce blood clots and stop bleeding- was also linked to a 100% R-OR.
“What this tells us is that, if possible, we should try to not match a recipient with obesity with a donor who has a history of alcohol use. If we can’t minimize the risk, then we’ll try to really manage the recipient’s coagulopathy- manage it more aggressively than if they didn’t have those risk factors,” said the principal investigator, Hunter Moore, MD, PhD.
Risks of Going Back to Operating Room
The Colorado Multi-Institutional Review Board study used liver transplant recipients who had signed up to collect blood samples prospectively during the first day after surgery.“We noticed a much higher rate of return to the operating room in certain populations, most patients with obesity,” Moore says. “We wanted to know if obesity was a real risk factor and what additional kind of factors was associated with it, and to see if any of those were modifiable to reduce the risk of needing a second operation.”
“During the transplant operation, the liver is a little slow and takes a while to wake up, which results in slow coagulopathic bleeding which causes blood to coagulate around it. It’s not very harmful, but when there’s a lot of it, it puts pressure on the liver and can slow its recovery," said Moore.
Risk Factors of a Liver Transplant
“The issues with returning to the OR are not really related to any detriment to survival and function,” Moore says. “But because it happens with one in four liver transplant patients, if you can reduce that number, it’s much better for patients’ recovery and it reduces the burden on OR staff.”The findings will help patients, their caregivers and surgical teams to plan for R-OR or possibly reduce risk before surgery.
“When I see my pre-evaluation liver transplant patients if they have a BMI that’s 30 or higher, I let them know that if they can work toward getting their BMI below 30 it may reduce their risks of returning to the OR and improve their outcomes,” Moore says. “Another way to mitigate risk is to fix coagulation in the OR aggressively. We can pre-emptively transfuse them with more hemostatic blood products if we know their coagulopathy risk before surgery.”
Risk factors more closely related to donors and donated livers will be the subject of future studies. Moore has started researching the enzyme transaminase levels in donor's livers, possibly linked to a higher risk of fluid accumulation in the abdomen after transplant surgery.
“One of our main goals is to understand risk factors so that we can anticipate outcomes and better plan for them during and after surgery,” Moore says.
Source-Medindia