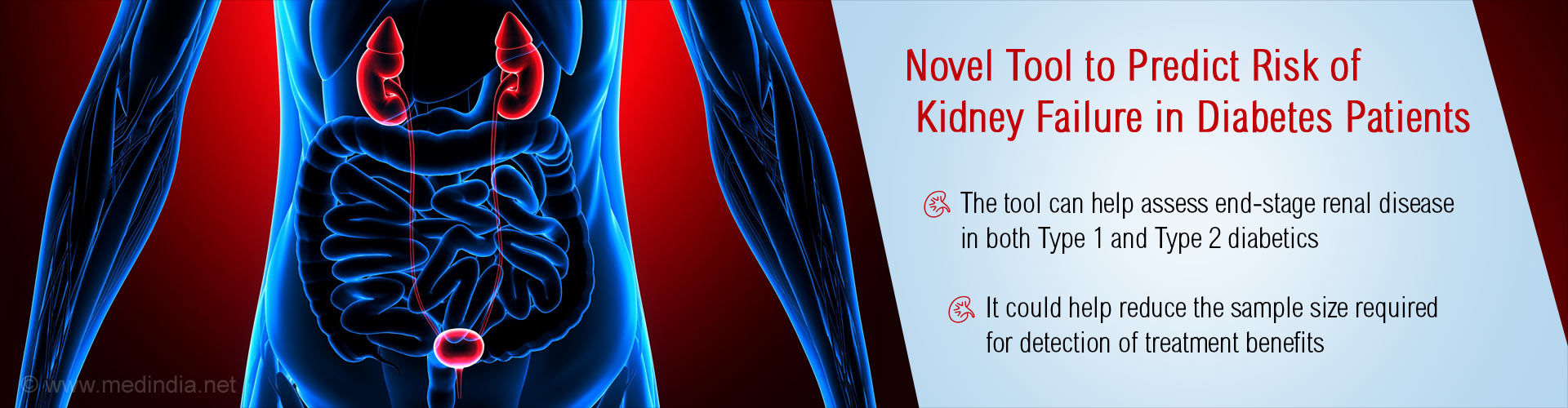
New analytic tool helps to identify specific values of two biomarkers, that indicate high risk of ESRD.
Highlights
- The previously used biomarkers in diabetes patients with end stage renal disease (ESRD) missed a large proportion of patients at high risk of the disease
- These biomarkers also failed to identify and enroll the right candidates for clinical trials, resulting in lack of useful information and decreased efficiency and cost-effectiveness.
- A new tool called the classification and regression trees (CARTs) helped to identify that specific values of two biomarkers, circulating level of TNFR1 and ACR combined, indicated high risk of ESRD in diabetics.
But these biomarkers missed a large proportion of patients who are at high risk of the disease and fail to predict the time of onset of ESRD.
"Overall efficiency and cost effectiveness of clinical trials depends on the diagnostic tools used to enroll study patients," says senior study author Andrzej S. Krolewski, M.D., Ph.D., Head, Section on Genetics & Epidemiology at Joslin Diabetes Center. "If you recruit people who are not at risk of progressing to ESRD during the clinical trial period, statistical power declines and you can't prove anything."
New Tool
Previously Dr. Krolewski and his team had discovered a link between tumor necrosis factor receptor 1 (TNFR1) and declining renal function in type 1 and type 2 diabetes.
An analytic tool called the classification and regression trees (CARTs) helped to identify that specific values of two biomarkers, circulating level of TNFR1 and ACR combined, indicated high risk of ESRD.
The prognostic criterion had a sensitivity value, which detected those at risk of ESRD, of 72% and, a positive prognostic value, which detected those who developed ESRD in three years, of 81%.
"Remarkably, when we used the TNF receptor to analyze risk of ESRD, the risk was almost identical for both type 1 and type 2 diabetes. This implies that the etiologies are similar," says Dr. Krolewski. "This is a very important observation because in the medical community, the impression is that the progression to ESRD in type 1 is somehow different from type 2. As a result, many clinical trials do not include patients with type 1."
Application of this criterion to enrollment in future clinical trials could reduce the sample size required to achieve adequate statistical power for detection of treatment benefits.
"Currently, about 80 percent of patients in these clinical trials provide no useful information," says Dr. Krolewski. "If our criterion is used in the recruitment of patients, you will not need two or three thousand patients for a clinical trial, you will only need 400 patients."
The findings are published in the online edition of Kidney International.
Reference
- Andrzej S. Krolewski et al. Improved clinical trial enrollment criterion to identify patients with diabetes at risk of end-stage renal disease. Kidney International; (year) doi.org/10.1016/j.kint.2017.02.010
Source-Medindia