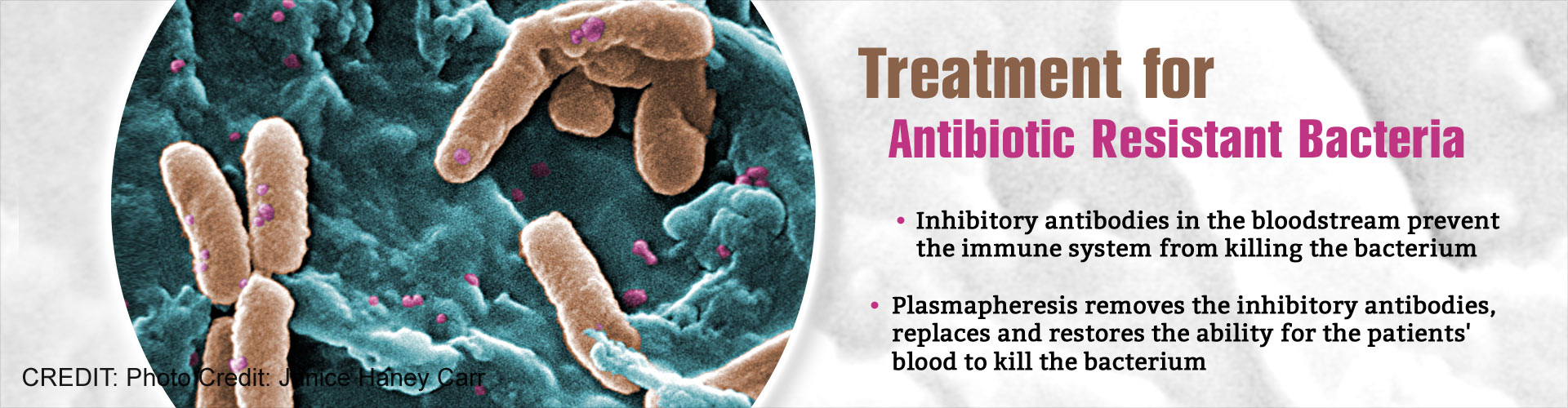
The process of removing antibodies from the blood stream, helps to treat antibiotic resistant bacteria and reduces the effects of chronic infections.
Highlights
- Two patients diagnosed with a debilitating lung condition, bronchiectasis, also simultaneously suffered from chronic Pseudomonas aeruginosa infection.
- These patients had an excess of a particular inhibitory antibody in the bloodstream, that stopped the immune system from killing the Pseudomonas aeruginosa bacterium and this worsened the patients' lung disease.
- Plasmapheresis was performed on both these patients that involved removing the antibodies from the blood stream and replacing them from blood donations, which restored the ability for the patients' blood to kill the infecting Pseudomonas.
- reduced the effects of chronic infections
- the number of days spent in hospital
- the need for use of antibiotics
One patient was a 64 year old male who had been diagnosed with the condition at 15 years of age, and the other was a 69 year old female, who had bronchiectasis from childhood.
Both the patients were housebound, required oxygen supplementation, nocturnal ventilation and did not respond to treatments.
Bronchiectasis is a debilitating disease that causes permanent enlargement of the airways in the lung. It is characterized by chronic cough, shortness of breath, coughing up blood, and chest pain.
In the U.K, it affects over 300,000 patients. Bronchiectasis often affects patients beyond the age at which lung transplantation is possible and this results in high mortality rate.
Chronic Pseudomonas aeruginosa lung infections commonly occur in patients suffering from bronchiectasis.
Professor Ian Henderson, Director of the Institute of Microbiology and Infection at the University of Birmingham said, "These patients had an excess of a particular antibody in the bloodstream. In contrast to the protective effect normally associated with antibody, in these patients the antibody stopped the immune system killing the Pseudomonas aeruginosa bacterium and this worsened the patients' lung disease. Perhaps counter-intuitively, we decided to remove this antibody from the bloodstream and the outcomes were wholly positive."
The patients had an excess amount of an inhibitory antibody that suppressed the immune response of killing the bacterium. They were subjected to plasmapheresis that involved the removal, treatment, and return of blood plasma from circulation. This was done 5 times in a week in order to remove the inhibitory antibody from the patients
Dr Tony De Soyza, Bronchiectasis service lead, Newcastle Upon Tyne Hospitals Trust and Senior Lecturer at Newcastle University said, "We needed a brand new way of tackling this problem. Working with kidney and immunology experts, we used a process known as plasmapheresis that is somewhat like kidney dialysis. The plasmapheresis involved the removal, treatment, and return of blood plasma from circulation, and was done 5 times in a week in order to remove antibody from the patients. We then replaced antibodies with those from blood donations. This treatment restored the ability for the patients' blood to kill their infecting Pseudomonas."
After the procedure was performed, both patients reported a rapid improvement in health and well-being, greater independence and improved mobility compared to any point in the previous two years.
Professor Henderson added "This shows that we can improve patient well-being significantly, by reducing the need for treatment and the numbers of days spent in hospital, which will also help to reduce the reliance on antibiotics. The next step is to do longer term studies to investigate whether an earlier intervention, with slightly less aggressive therapies, could help prevent disease progression in patients."
This study is the first to describe the antibody-dependent enhancement of bacterial disease.
It could be applicable to other bacterial infections and offers hope for the treatment of some antibiotic resistant infections.
The study is published in the American Journal of Respiratory and Critical Care Medicine.
Reference
- Ian Henderson et al. The Use of Plasmapheresis in Patients with Bronchiectasis with Pseudomonas aeruginosa Infection and Inhibitory Antibodies. American Journal of Respiratory and Critical Care Medicine; (2017) doi.org/10.1164/rccm.201603-0599LE
Source-Medindia