Study shows that the nature of retinopathy of prematurity care is being gradually transformed by recent advancement in technologies.
- Retinopathy of prematurity is the most common cause of visual loss in childhood, especially in countries lacking in trained staffing and functional equipment.
- Advancement in technology and their implementation, has improved the nature of care for ROP in the form of early detection and treatment.
- One such option is the use of telemedicine for the detection of ROP especially in areas in which trained examiners are not available.
This is one of the most common causes of visual loss in childhood and can lead to lifelong vision impairment and blindness.
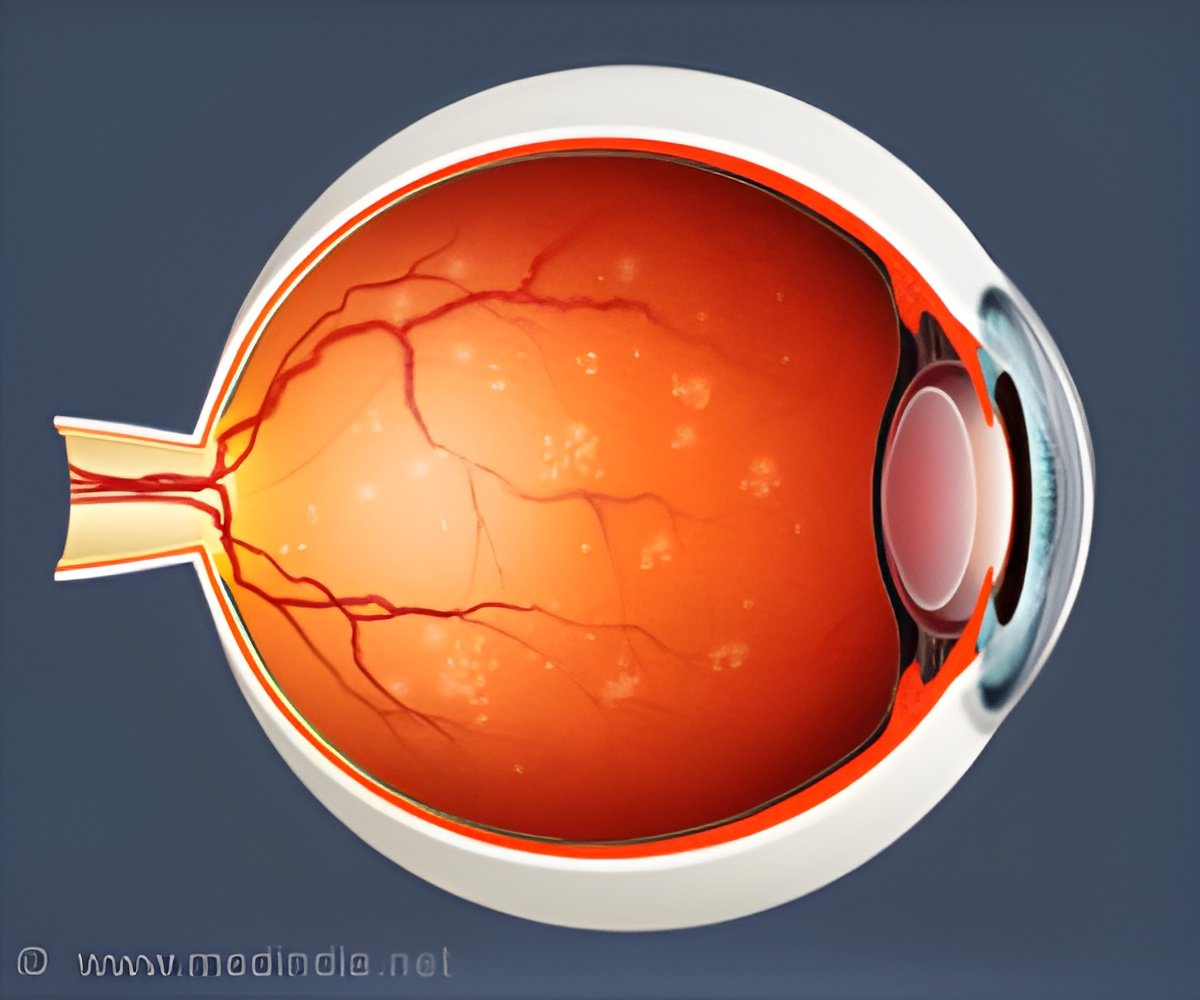
ROP occurs when abnormal blood vessels grow and spread through the retina, potentially leading to retinal detachment and blindness.
There has been improvements in the lives of patients suffering from this condition, due to advances in diagnosis, management, and prevention of ROP
In Western countries, more than 90% of premature infants even with severe ROP can expect a favorable outcome.
ROP will continue to be a leading cause of blindness among infants if there is shortage of more accessible treatments.
Among them 90% of those affected have only mild disease and around 1,100- 1,500 develop disease severe enough to require medical treatment.
Around 400-600 infants each year in the U.S. become legally blind from ROP.
Telemedicine
ROP is traditionally treated using laser ablation of the abnormal blood vessels, but advancements have been made using vascular endothelial growth factor (VEGF) inhibitors.
One proposed solution is the use of telemedicine for the detection of ROP especially in areas in which trained examiners are not available.
Making use of wide-angle retinal imaging, computing, and information technology have facilitated the implementation of major real-world telemedicine programs for the treatment of ROP in the United States and throughout the world.
According to Dr. Michael F. Chiang, MD, of the Departments of Ophthalmology & Medical Informatics and Clinical Epidemiology, Casey Eye Institute, Oregon Health & Science University, Portland, OR, "The nature of ROP care is now being gradually transformed by some of these technologies. By evaluating other emerging imaging technologies, understanding their benefits and limitations, and gradually implementing them into practice when warranted, pediatric ophthalmologists will be able to enhance the care they provide to patients for a broader range of problems in the future."
Helen A. Mintz-Hittner, MD, Department of Ophthalmology and Visual Science, University of Texas Health Science Center-Houston, McGovern Medical School, Houston, TX, has worked on bevacizumab that has revolutionized the way many physicians treat advanced ROP.
Though the treatment shows promise, a delayed recurrence of ROP after bevacizumab treatments does occur usually at 5-10%)
Dr. Mintz-Hittner emphasizes "the need for proper case selection (timing), careful injection (technique), and appropriate long-term follow-up (at least 65 weeks adjusted age) for parameters (outcomes)" to properly manage an ROP infant.
David K. Wallace, MD, MPH, of the Departments of Ophthalmology and Pediatrics, Duke University School of Medicine, Durham, NC, says "we have a long way to go to have an evidence-based paradigm for anti-VEGF treatment. There are many unanswered questions about which drug, what dose, relative benefits, and possible side effects. Consequently, there are many opportunities for high-quality comparative studies that will shape our future treatment of premature infants and aid in reducing the burden of blindness from ROP."
The findings are published in the Journal of the American Association for Pediatric Ophthalmology and Strabismus (AAPOS).
Reference
- Retinopathy of Prematurity - (https://www.aapos.org/terms/conditions/94)
Source-Medindia