Men with metastatic melanoma have a better survival rate if they are obese as they respond better to immunotherapy.
Highlights
- Obese men with melanoma or skin cancer have a better survival rate than those with a normal BMI.
- Usually, women are at a lower risk due to the increased production of estrogen that responds well to immunotherapy that helps kill cancer cells.
- Obese men also have high levels of estrogen as the adipose tissue converts androgens to estrogens and poses the same effect to immunotherapy.
"The question is what underlying mechanism causes this advantage in obese men, and can we take advantage of it to improve outcomes in patients with melanoma?" McQuade said. "One hint may be the interaction between obesity, sex, and outcomes, which has not been detected before in any cancer."
Women with metastatic melanoma have long been known to have better outcomes compared to men, McQuade noted. In this study obesity overcame that survival disadvantage for men, leading researchers to now look at the possible impact of sex hormones in this effect.
How Does Obesity Increase Survival Rate?
The relationship between obesity and survival in patients that already have cancer is not as consistent. Recent studies have shown a similar survival benefit for obese patients with colorectal or kidney cancer.
The team expected to find obesity to be harmful for melanoma patients, based in part on research that implicates obesity in activation of a cancer-promoting molecular pathway called IGF-1/PI3K/AKT.
While advantages in PFS and OS emerged in an overall meta-analysis of the entire group, the survival benefit associated with obesity was restricted to men treated with targeted or immunotherapies, where obese men had a 47 percent decreased risk of death compared to men with normal BMI.
Overall survival in men
The results from 599 patients receiving combination targeted therapy of dabrafenib (BRAF inhibitor) and trametinib (MEK inhibitor) show that :
- Those with normal BMI of 18.5-24.9kg/m2 had a PFS of 9.6 months, OS of 19.8 months.
- Those who are obese with a BMI 30 and above had a PFS of 15.7 months, OS of 33.0 months.
- Even after including factors such as age, sex, stage, disease burden, certain mutations and prior treatment showed that obesity still improved PFS and OS compared to normal BMI patients.
- By contrast, women, for example, had overall median survival of at least 33 months, regardless of BMI.
Obesity is associated with increased inflammation, which could improve the effectiveness of checkpoint blockade drugs that unleash an immune response against cancer.
The sex-specificity of the observed differences points to a potential hormonal mediator. Fat (adipose) tissue produces an enzyme called aromatase that converts male hormones called androgens into estrogens, female hormones. Perhaps this happens enough in obese men to help them clear some type of hurdle toward greater survival, McQuade said.
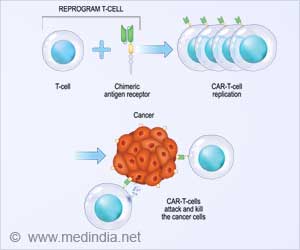
The researchers are collaborating with investigators at the University of Pennsylvania that have found that turning on a very specific type of estrogen receptor on melanoma makes it vulnerable to immunotherapy.
The MD Anderson team also is looking at gene expression, mutations and immune profiling to identify potential differences in melanoma in obese and non-obese patients and developing preclinical models.
Source-Medindia