Researchers find that there is substantial geographic variation in access to kidney transplantation, with a disproportionate lack of access in the Southeast U.S.
Unlike dialysis which is performed routinely, kidney transplantation is done when a suitable donor kidney is found and you don’t have any new medical problems. You will have to go through various assessments and lab tests, and when the surgery team finds that the donor kidney is in good condition and suitable for you, they will quickly prepare you for the surgery.
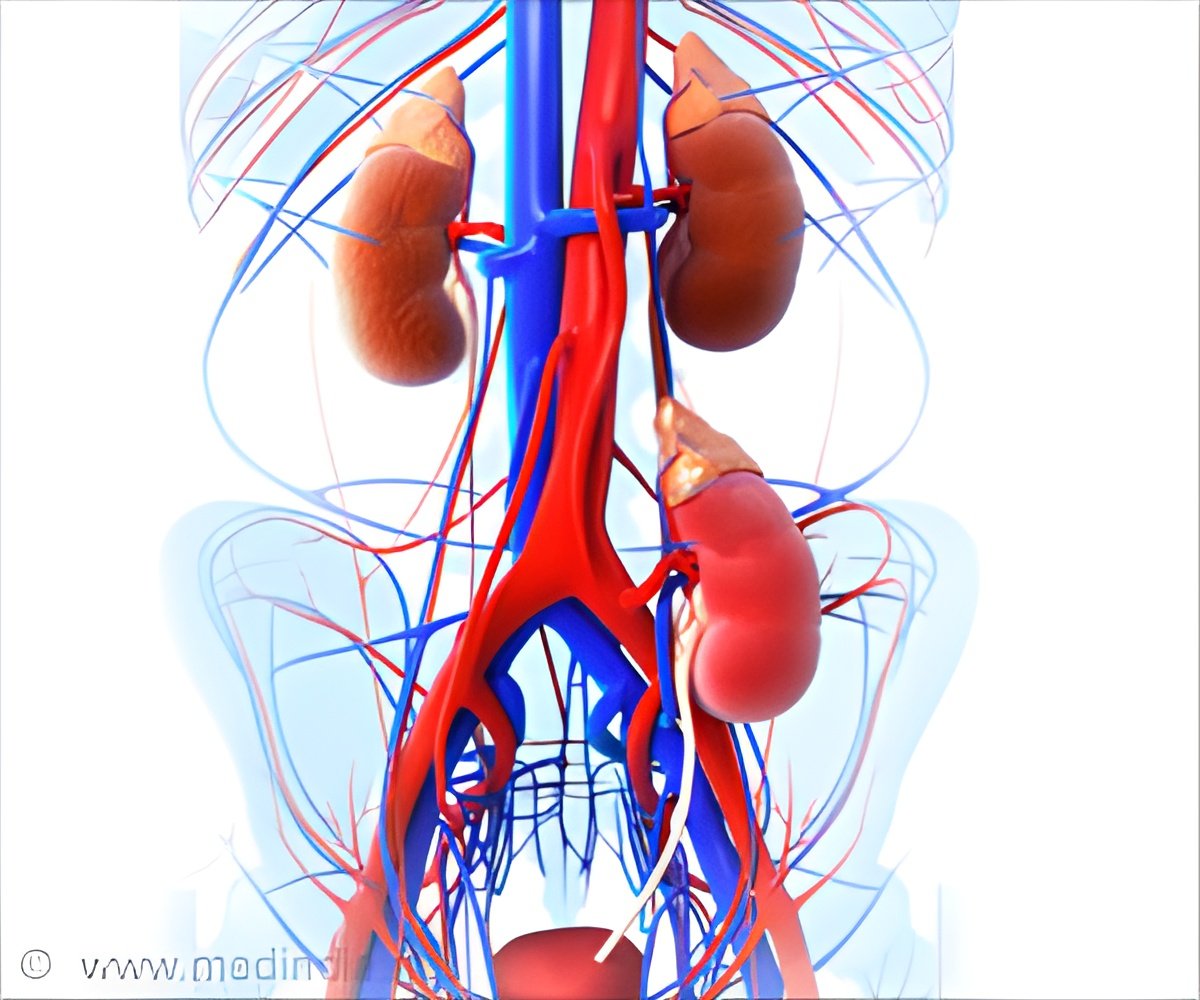
The Kidney Transplant Procedure is as follows:
• The diseased kidney is left as it is unless it is causing pain or is infected.
• An incision is made in your lower abdomen to the front.
• Blood vessels from your lower abdomen are connected to the blood vessels of the donated kidney.
• A stent may be inserted in the ureter to ensure a good flow of urine. The stent is removed in 6 to 10 weeks through a procedure called cystoscopy.
Regional Disparities in Kidney Transplantation Access
Unfortunately, all ERSD patients in the United States do not have access to kidney transplantation, though there are more than 4000 dialysis facilities. Dr. Rachel Patzer and her team at the Emory University School of Medicine found that there is substantial geographic variation in access to kidney transplantation, with a disproportionate lack of access in the Southeast. Southeastern region includes the states of Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, Tennessee, and Virginia.
The research team looked for characteristics of dialysis facilities that were linked with delayed access to kidney transplantation. They found that the following had lower rates of kidney transplantation:
• African American patients
• Uninsured patients
• Patients with diabetes
• Profit making companies
• Facilities with fewer staff
The lowest performing dialysis facilities were in the Southeast and the highest in the Northeast. Poverty is the main reason for this inequity, the researchers found.
‘The disparities that we have reported in access to kidney transplantation within dialysis facilities in the Southeastern US are linked to the higher concentration of poverty in this area of the country compared to other regions,’ said Dr. Patzer.
The researchers offered various strategies to address the disparities in access to kidney transplantation. For example, they suggested that:
• Low performing facilities could focus on internal quality improvement activities
• Making policy changes to increase staffing
• Standardizing patient education
• Expanding Medicaid eligibility
Titte Srinivas, MD, of the Medical University of South Carolina, notes that the inequity in access among kidney failure patients in the Southeast reflects the ‘interaction of patients' socioeconomic and biologic factors with the financial and organizational structure of the healthcare system’. Poverty and lack of education are the main barriers to the access of kidney transplantation, according to him.
It is also a reflection of population health since organ donation from living donors is limited by the health of the donor population. Dr Srinivas suggested the need to use ‘top-down’ approach in the health care delivery system to improve the population health in the Southeast.
Racial Disparities in Access to Kidney Transplantation
In another study published in the American Journal of Transplantation, Dr Rachel Patzer and her team found that black patients had a 59 percent lower rate of transplantation over that of white patients. The study examined 2,291 patients, nearly two-thirds of whom were black and a third lived in low-income areas, to determine the effect of race on referral, evaluation, wait-listing, and organ transplantation.
‘Despite near-universal health care coverage for end-stage renal disease (ESRD) patients through the Medicare ESRD program, black ESRD patients are at a disadvantage to receive kidney transplantation,’ Dr. Patzer reported. ‘Socioeconomic status really accounts for about 30% of this observed racial disparity in transplant access.’
She suggested that patient education may help reduce racial disparities in access to kidney transplantation.
Ultimately, whether it is the regional disparity or racial disparity, socioeconomic status of the ESRD patient is the main barrier to the access of kidney transplantation.
Source-Medindia














