A testosterone-related genetic abnormality can help predict patients’ responses to specific prostate cancer therapies, a study at Cleveland Clinic found.
- Testosterone-related genetic abnormality can help predict treatment outcome in prostate cancer.
- Men who inherit this genetic abnormality need personalized treatment.
- Traditional radiation therapy does not prevent recurrence of prostate cancer.
Back-to-back discoveries from Cleveland Clinic demonstrate for the first time how a testosterone-related genetic abnormality can help predict individual patient responses to specific prostate cancer therapies. The studies suggest that men who inherit this variant would benefit from a personalized treatment plan that targets specific hormonal pathways.
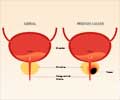
Recurrence of prostate cancer after radiation therapy
ADT works by blocking prostate cancer's supply of male hormones in the testes. It is a cornerstone treatment for recurrent prostate cancer, but it often stops working, allowing cancer to progress and spread. In 2013, Dr. Sharifi discovered that prostate cancer cells with the genetic abnormality survive ADT by producing their own androgens.
In the first new study, Dr. Sharifi and colleagues from Memorial Sloan Kettering Cancer Center, Harvard/Dana-Farber Cancer Institute and University of Michigan Comprehensive Cancer Center analyzed 213 men whose prostate cancer recurred after radiation therapy and underwent ADT. They found for the first time that following radiation and ADT, prostate cancer was much more likely to spread--and spread rapidly--in men who had the HSD3B1(1245C) variant.
The second study, performed in collaboration with researchers at University of California San Francisco, examined a group of 90 men with metastatic cancer that had become resistant to ADT. These patients were subsequently treated with the drug ketoconazole, which blocks the production of androgens outside of the testes (e.g., those developed by prostate cancer cells that are evading ADT treatment).
New Target for Treatment
Surprisingly, men with the genetic anomaly fared better on ketoconazole than men without the variant. This finding raises the possibility that targeting variant tumors' backup androgen supply (outside of the testes) could be a successful strategy when ADT fails.
These discoveries complement earlier studies and support the use of HSD3B1(1245C) as a predictive biomarker to help guide critical treatment decisions. While the outlook of patients with this gene variant is poor, these studies offer hope for a new treatment strategy for these men, and more studies are needed using next-generation androgen inhibitors, such as abiraterone and enzalutamide.
Dr. Sharifi is also a member of the Glickman Urological and Kidney Institute and Taussig Cancer Institute of Cleveland Clinic. He holds the Kendrick Family Chair for Prostate Cancer Research at Cleveland Clinic and co-directs Cleveland Clinic's Center of Excellence for Prostate Cancer Research. In 2017 he received a Top Ten Clinical Research Achievement award from the Clinical Research Forum for his landmark discovery that men who carry the HSD3B1(1245C) variant are more likely to die from their disease.
References:
- W. Hahn, MD, Sumanta K. Pal, MD; Neeraj Agarwal, MD. HSD3B1 - A Predictive Biomarker in Advanced Prostate Cancer, JAMA Oncology https://jamanetwork.com/journals/jamaoncology/article-abstract/2657133