-Using the right combination halotypes will help in producing an embryo that is free of disease-causing genetic mutations.
- Children inherit mutated mitochondrial DNA from mothers, which can sometimes be fatal.
- Mitochondrial replacement therapy offers an effective way of replacing the faulty //mitochondria with those from a healthy donor.
Mitochondrial replacement therapy has been approved for clinical trials in the United Kingdom.
Similar group of mitochondrial DNA are known as halotypes. Each halotypes represent major branching points on the human genetic family tree.
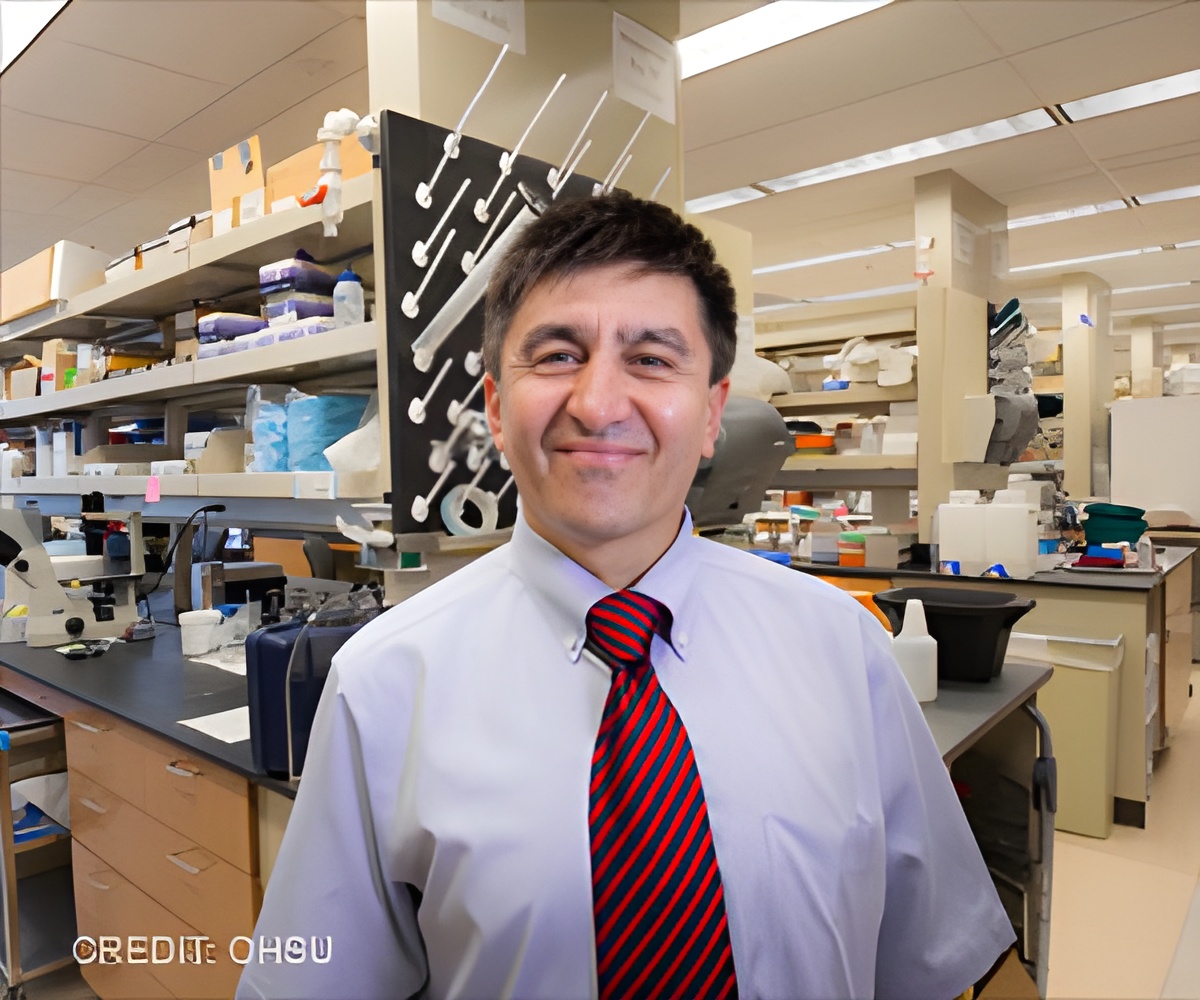
Researchers led by Shoukhrat Mitalipov, Ph.D. are studying how to conduct mitochondrial replacement therapy in a safe way to prevent the transmission of harmful mutant mitochondrial DNA from mothers to children.
"This research suggests that we're going to have the greatest success rates for producing an embryo free of disease-causing genetic mutations by making sure we are using the right combination of haplotypes," said senior author Shoukhrat Mitalipov, Ph.D., who directs the Center for Embryonic Cell and Gene Therapy at OHSU.
Spindle-Transfer Technique
This technique has a small glitch as even a small amount of mutant mitochondrial DNA transferred with the mother's nucleus can replicate quickly as the embryo develops and cause the disease.
Choosing Healthy Donors
For the current research, Mitalipov and colleagues recruited four families who have children suffering from Leigh Syndrome and one with a neurodegenerative disorder called MELAS.
Donor eggs from 11 healthy women were collected and screened to confirm that they did not carry inherited pathogenic mutations in their mtDNA.
Spindles from carrier eggs were transferred into 36 donor eggs stripped of their nuclei. They were fertilized, cultured to blastocysts, and subsequently to embryonic stem cell lines.
Most stem cells developed with the donor's healthy mitochondrial DNA continuing to dominate.
But a few stem cell lines displayed gradual return to the mutant maternal mtDNA. As those stem cell lines continued to grow in the laboratory, they reverted completely to the original maternal mitochondrial DNA.
The Reason for Reverting to Mutant Maternal mtDNA-
"Currently, there is a lack of studies on the efficacy and safety of oocytes derived from women carrying pathogenic mtDNA mutations," said co-author Juan Carlos Izpisua Belmonte, Ph.D., with the Salk Institute for Biological Studies in La Jolla, California. "Our study fills the gap."
When researchers identified a portion of the mtDNA known as the D-loop, which initiates replication of the entire genetic sequence, they discovered DNA code polymorphisms that result in preferential replication of the mother's mtDNA.
In order to conduct mitochondrial replacement therapy at clinical levels, researchers are proposing careful selection of donor mitochondria to avoid a return of mutant mitochondria.
Source-Medindia