Sleep apnea during pregnancy is associated with increased post-delivery risk of hypertension and metabolic syndrome.
- Sleep apnea during pregnancy increases post-delivery risk of hypertension and metabolic syndrome
- High blood pressure during pregnancy can lead to serious health consequences
- Using simple oxygen monitoring devices can help identify women who are at risk early
Participants were a subgroup of 1,964 women who were part of the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-be Heart Health Study (nuMoM2b-HHS) and were experiencing their first pregnancy, and 1,222 of the same study participants who were examined 2-7 years after delivery. The researchers then determined whether participants were at increased risk for hypertension or metabolic syndrome.
“While epidemiologic data from cohorts of middle-aged and older adults indicate that sleep disordered breathing is associated with adverse cardiometabolic outcomes, less is known about how sleep-disordered breathing in pregnancy and in the post-delivery period impacts maternal health,” stated the authors.
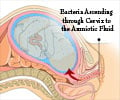
Sleep disordered breathing during pregnancy has been associated with a two to three-fold increased risk for preeclampsia—persistent high blood pressure during pregnancy that can lead to serious health consequences—and/or gestational diabetes (diabetes that develops during pregnancy). These and other adverse pregnancy outcomes are risk factors for later development of hypertension and metabolic disease in the mother.
Study participants were tested both during pregnancy and two to seven years later, each using the same model home sleep apnea test. Among other factors, sleep apnea tests measure the number of times a person experiences breathing pauses and associated drops in oxygen levels.
“We found that the presence of sleep apnea measured both during pregnancy and two to seven years after delivery was associated with the development of hypertension and metabolic syndrome,” said Dr. Facco.
Incident hypertension is defined as the first occurrence at any follow-up visit of systolic blood pressure 140 mm HG or higher or diastolic blood pressure 90 mm HG or higher.
“Our data also demonstrated a higher risk of developing metabolic syndrome and hypertension using a simple measurement of oxygen dips per hour of sleep,” said study co-author Susan Redline, MD, MPH, who directs the Sleep Medicine Epidemiology program at Brigham and Women’s Hospital and Harvard Medical School, Boston.
“These results suggest that use of simple oxygen monitoring devices may be useful for identifying women in pregnancy and in the post-delivery period at risk for adverse health outcomes and identifying women who may potentially benefit from treating sleep apnea.”
“These data underscore the need to rigorously evaluate the role of screening and treating sleep apnea during pregnancy and in the post-delivery period as new strategies for early interventions aimed at improving long-term maternal health,” the authors concluded.
Source-Eurekalert