Study assesses the independence of associations among uric acid concentrations, fructose consumption, and nonalcoholic steatohepatitis confirmed by biopsy.
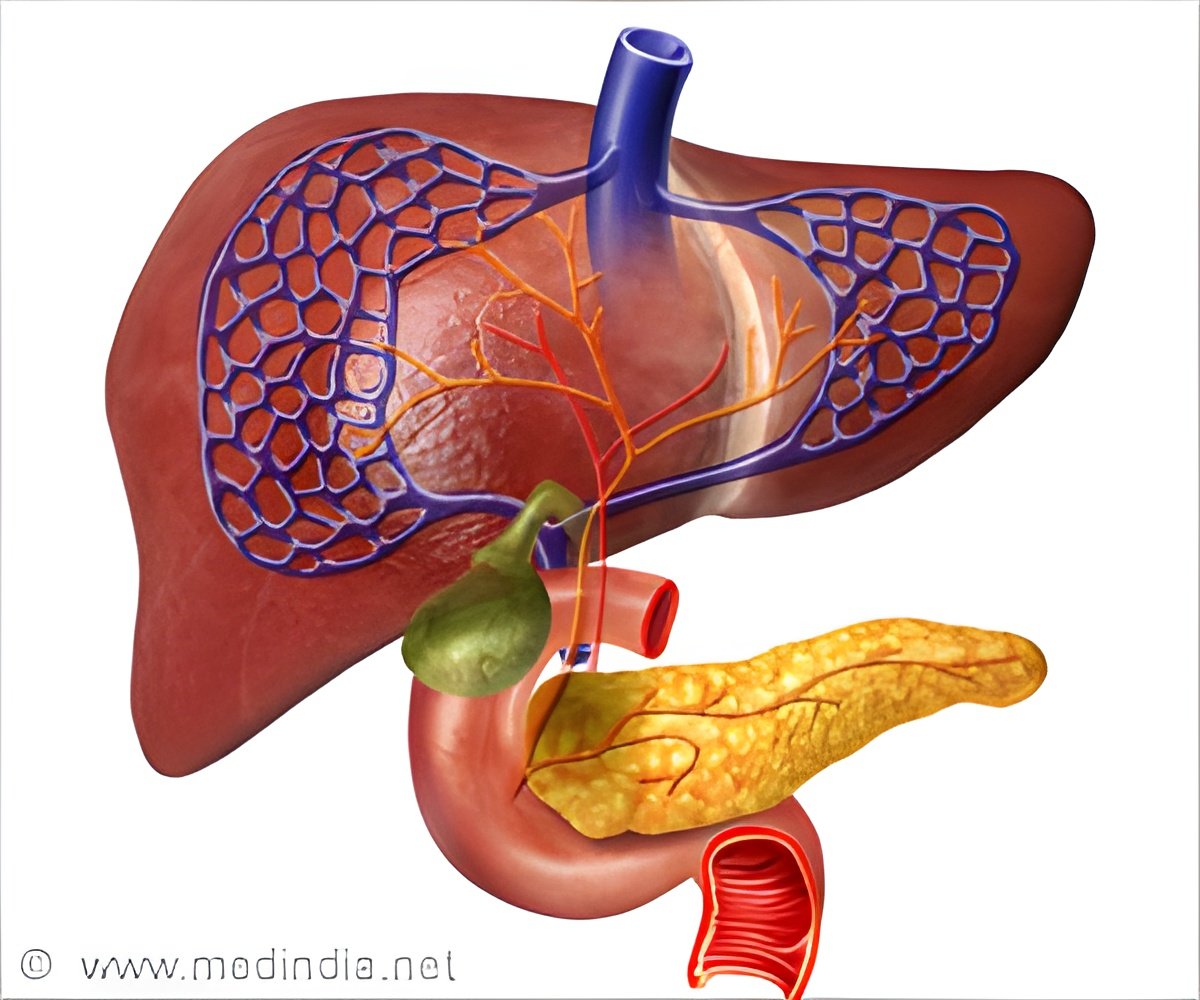
- Nonalcoholic steatohepatitis (NASH) is a type of non-alcoholic fatty liver disease.
- NASH affects life expectancy and quality of life and therefore it is important to understand the risk factors for NASH in children and adolescents.
- Study states that sugar (fructose) intake and uric acid concentration are the main risk factors for NASH that independently contribute to the incidence and progression of liver disease, mainly non-alcoholic steatohepatitis(NASH).
NAFLD, is the accumulation of extra fat in liver cells in people who drink little or no alcohol. It is the fastest growing cause of liver disease in both Western and developing countries.
Nonalcoholic steatohepatitis (NASH) is a type of NAFLD. In NASH there is inflammation and liver cell damage, in addition to fat accumulation in the liver.
Around 30%-40% of the general population in United States have NAFLD and 3%-12% of adults in U.S have NASH. About 20% of people with NAFLD have NASH.
Up to 9.6% of all children and 38% of obese children are affected by NAFLD, including NASH.
"It is plausible that dietary fructose intake and uric acid concentrations are potential risk factors for liver disease progression in NAFLD. Numerous studies have shown that high uric acid levels are associated with metabolic syndrome and NAFLD, but to date, to the best of our knowledge, no studies have tested the independence of associations among uric acid concentrations, fructose consumption, and NASH confirmed by biopsy," explained senior investigator Valerio Nobili, MD, Chief of the Hepatometabolic Unit Liver Diseases Laboratory, Bambino Gesù Hospital, IRCCS, Rome, Italy.
A team of researchers in Italy and the UK studied 271 obese children and adolescents with NAFLD among whom 155 were males with mean age 12.5 years. They had undergone liver biopsy.
The participants completed a food frequency questionnaire, indicating :
- when specific foods were consumed (breakfast, morning snack, lunch, afternoon snack, dinner, etc.)
- how often (every day of the week, sometimes, or never)
- portion size
Nearly 90% reported drinking sodas and soft drinks one or more times a week. Almost 95% of patients regularly consumed morning and afternoon snacks consisting of crackers, pizza and salty food, biscuits, yogurt, or other snacks.
Results showed that 37.6% of patients had NASH and 47% of patients with NASH had high uric acid compared with 29.7% of patients who did not have NASH.
Fructose consumption was independently associated with high uric acid, which occurred more frequently in patients with NASH than in not-NASH patients.
"In this study, we show for the first time that uric acid concentrations and dietary fructose consumption are independently and positively associated with NASH. The development of NASH may markedly affect life expectancy and quality of life in affected individuals and therefore it is crucial to understand the risk factors for NASH in children and adolescents in order to design effective interventions which can be used safely to treat this young group of patients," Dr. Nobili concluded.
Fructose consumption can be reduces by directing efforts towards behavior modification, nutrition education, and limiting access to soda and other sweetened beverages. Many countries have already launched campaigns to ban soda vending machines in schools.
Thus the results state that both dietary fructose consumption and serum uric acid concentrations independently contribute to non-alcoholic steatohepatitis (NASH) and its progression.
The findings are published in the Journal of Hepatology.
References
- Definition & Facts of NAFLD & NASH(NASH) - (https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/definition-facts
- Valerio Nobili et al. Serum uric acid concentrations and fructose consumption are independently associated with NASH in children and adolescents. Journal of Hepatology; (2017) doi.org/10.1016/j.jhep.2016.12.025
Source-Medindia












