Mitochondria or powerhouses of the cell could be a good treatment strategy for recovery from a stroke of brain injury.
- Mitochondria supplies the energy needed for cells to live and function and also trigger cell death or apoptosis.
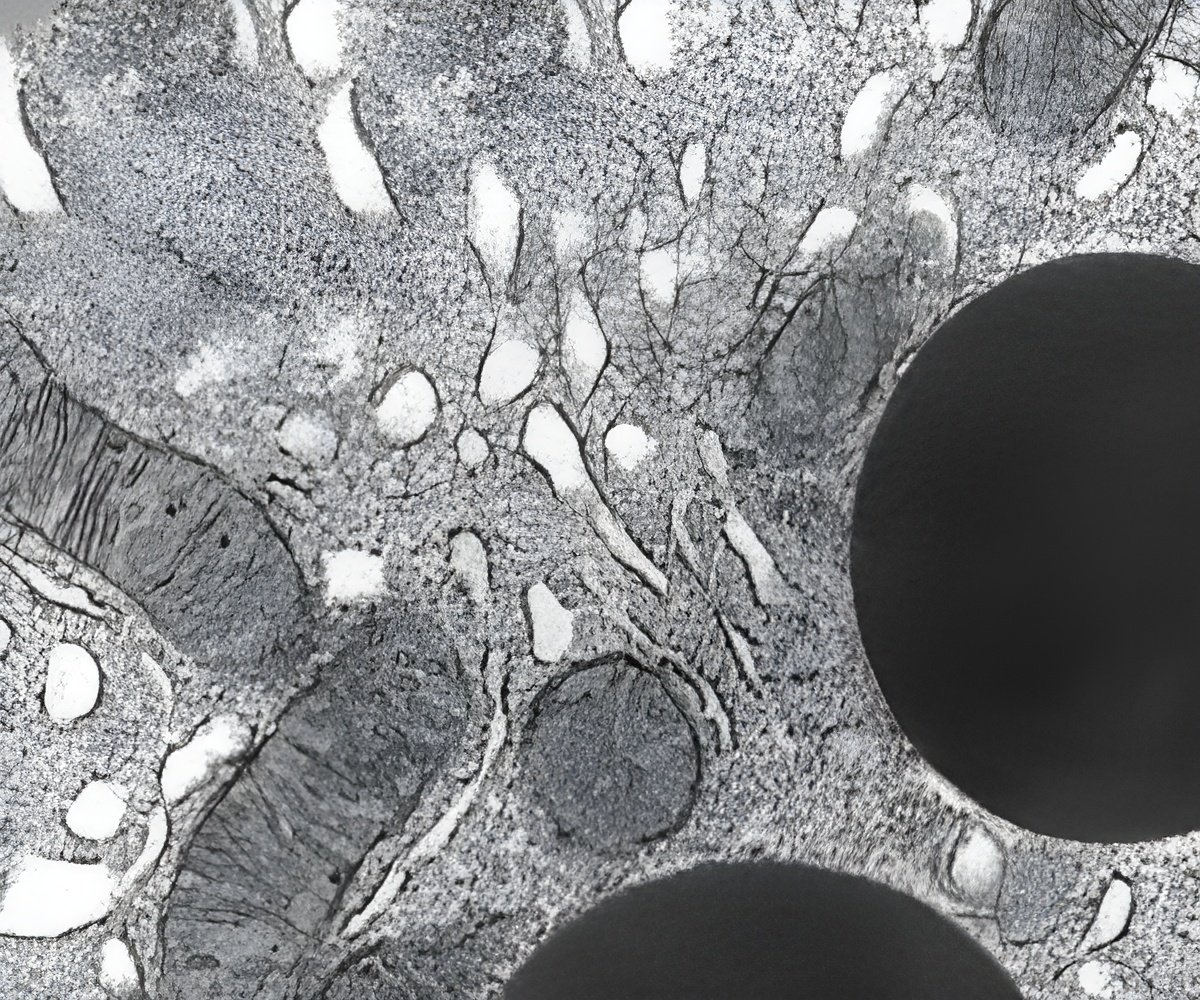
- Their function depends on their shape, where healthy mitochondria are long and lean and dysfunctional mitochondria are thick and fragmented.
- Stroke or brain injury leads to fragmentation of mitochondria, following which they fail to perform their protective functions.
- New study states that mitochondria can be a potential target for therapeutic interventions following stroke or brain injury.
Neurons and muscle cells have more mitochondria compared to any other cells in the body because they are two of the biggest energy users.
In a healthy brain scenario, if mitochondria happen to create too many new mitochondria, they will recycle them just like they do with old ones they replace.
Following a brain injury or events like cardiac arrest which is considered as global ischemia, where the entire body is deprived of oxygen, the mitochondria often resume their long and lean shape with time once blood and oxygen are restored to mild or moderately damaged tissue.
But the supply of oxygen or blood should be within 5 minutes following the incident. If the delay occurs by extra three minutes, mitochondria does not regain their usual high-functioning lean state.
Mitochondria functions by either protecting neurons by supplying ATP (adenosine triphosphate) and adsorbing excessive calcium ions, or killing neurons by releasing pro-apoptotic factors.
- healthy mitochondria are thin and long
- dysfunctional mitochondria are thick (swollen) and short (fragmented)
Mitochondria are dynamic structures that are connected to each other and can maneuver around a dendrite to support the point of highest energy need at that moment.
They supply energy needed for cells to live and function but can also trigger cell death or apoptosis.
Mitochondria protect cells is by capturing calcium, an important signaling molecule in the brain and supplying ATP (adenosine triphosphate).
During a brain injury mitochondria become injured or fragmented and trigger deadly signals.
They cannot perform protective functions of capturing calcium anymore. This may result in excess levels of calcium which can be lethal and lead to cell death.
Studying the 'Powerhouses' in Real-Time
Researchers studied the fragmented mitochondria in transgenic mice with brain injury.
They used two-photon laser scanning microscopy to document the cell powerhouses in the minutes, hours and days after mild, moderate and severe injury.
One of the first areas to be affected by stroke or brain injury is the cortex, which is associated with higher cognitive functions.
The cortex has pyramid shaped neurons with long and lean dendrites. They constantly receive signal from other neurons and are packed with mitochondria.
During a stroke or injury, these neurons become fragmented and the researchers discovered that the destructive mitochondrial transformation actually happened first and within minutes.
So intervening at the mitochondrial level within a short duration following a stroke or brain injury may aid in recover.
Work Ahead for Researchers
Mitochondria can split and form new mitochondria to replace old ones. As part of recovering from severe injury, scientists need to determine whether these are actually new mitochondria emerging after a prolonged recovery from severe injury or if they are repaired ones.
Researchers also want to look at energy output of recovered mitochondria and existing drugs that might enhance that recovery.
Kirov and Dr. Leonard Khiroug, neuroscientist at the Neuroscience Center at the University of Helsinki, Finland, are co-corresponding authors of the work in living brains published in the Journal of Neuroscience.
Reference
- Sergei A. Kirov et al. Reversible disruption of neuronal mitochondria by ischemic and traumatic injury revealed by quantitative two-photon imaging in the neocortex of anesthetized mice. Journal of Neuroscience ; (2016) DOI: https://doi.org/10.1523/JNEUROSCI.1510-16.2016
Source-Medindia