- Policy Evolution: Recent shifts in India’s health policy emphasize private insurance schemes over strengthening public sector care
- Healthcare Disparities: Public health needs vary from poverty-related illnesses to chronic diseases, with differing impacts on various social groups
- Trust Issues: The focus on privatization has weakened trust in the public health system and necessitates a balance between private and public care
Public Health as a Problem-Solving Activity: Barriers to Effective Action
Go to source).
The reliance on private healthcare has intensified inequalities in access, leaving many dependent on costly treatments. medindia publichealth’
Types of Public Health Needs
Public health needs can be categorized into three primary groups.- The first group includes diseases linked to poverty, such as tuberculosis, malaria, and undernutrition, which disproportionately affect the poor. These health issues are intertwined with broader socioeconomic factors like poor sanitation and limited access to clean water. Effective public health policies must address both health conditions and their underlying causes, such as livelihoods and access to resources, to truly improve public health outcomes.
- The second group encompasses the health issues faced by the middle class and wealthier sections of society. Problems like environmental pollution, lack of proper waste management, and rising rates of chronic diseases are often attributed to poor infrastructure and inadequate market regulation. These concerns, while important, tend to receive less attention in public health policies despite their significant impact on quality of life.
- The third group focuses on curative care, which is a critical aspect of public health. The provision of primary, secondary, and tertiary care is essential for addressing the curative needs of the population. However, primary healthcare, which serves as the backbone for the poor and vulnerable, often struggles with inadequate infrastructure and a shortage of medical professionals. While government initiatives like the Pradhan Mantri Jan Arogya Yojana (PMJAY) aim to provide tertiary care for the poor, secondary-level care remains neglected.
Evolution of India’s Public Health Policies
In recent years, public health policy in India has undergone significant changes. The launch of the National Rural Health Mission (NRHM) in 2005, followed by the National Health Mission (NHM) in 2013, marked a departure from the earlier National Health Policy of 2002, which leaned towards the commercialization of healthcare. The NHM aimed to strengthen public sector healthcare through a focus on primary healthcare and national health programs.However, since 2018, there has been a shift in focus towards Publicly Funded Health Insurance schemes (PFHI), such as the PMJAY under Ayushman Bharat. These schemes, while offering hospital coverage to a select segment of the population, have been criticized for outsourcing secondary and tertiary care to the private sector at market rates. This has led to concerns that public health policies are favoring private healthcare providers, leaving a significant portion of the population dependent on expensive, commercialized care.
Private Sector Dominance in Healthcare
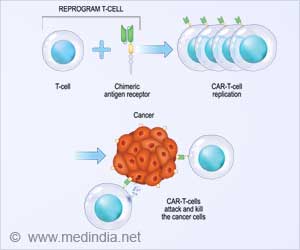
The PFHI schemes have inadvertently benefited private healthcare providers more than the public sector.By covering only hospital expenses, these schemes leave a vast portion of healthcare costs uncovered, forcing many to seek expensive private care. Additionally, the government’s outsourcing of secondary and tertiary care to private hospitals at market rates is seen as an acknowledgment of the inadequacies in public sector healthcare. This reliance on private providers not only limits access for those outside the insurance schemes but also weakens the public health system by diverting resources away from much-needed infrastructure development.
The Controversy Surrounding Health and Wellness Centres (HWCs)
Another significant policy shift occurred in 2018 with the transformation of sub-centers, primary health centers (PHCs), and community health centers (CHCs) into Health and Wellness Centres (HWCs).These centers were established to provide curative care, but the move has been criticized for undermining the original mandate of these institutions, which focused on preventive and outreach activities. Additionally, the introduction of community health officers with limited medical training has raised concerns about the quality of care being provided in these centers.
The recent decision to rename these centers as ‘Ayushman Arogya Mandirs’ has sparked further controversy. The name change, with its religious connotations, has raised questions about its appropriateness in a secular healthcare system, particularly in non-Hindi speaking regions.
The Need for Balanced Health Policy Approach
Public health policy management must consider the diverse needs of the population, ensuring that all social groups receive adequate attention.For the poor and vulnerable, access to primary and secondary curative care remains a critical need. Strengthening the public health infrastructure and ensuring adequate staffing in healthcare facilities should be a priority.
Meanwhile, addressing the health issues of the middle class, such as pollution and chronic diseases, requires a focus on long-term solutions, including better infrastructure and regulatory measures.
The current trend towards privatization and insurance-based schemes risks exacerbating inequalities in access to healthcare. A balanced approach that strengthens public sector healthcare while addressing the needs of all population groups is essential for building a resilient and equitable public health system.
Restoring Trust in Public Healthcare
Public health policy management in India faces significant challenges, including a lack of investment in secondary and tertiary care in the public sector. The emphasis on publicly funded insurance schemes, coupled with the weakening of primary healthcare institutions, has eroded public trust in the system. To restore confidence in public healthcare, policymakers must prioritize strengthening the public health infrastructure, ensuring that primary, secondary, and tertiary care needs are met for all sections of society.Addressing the diverse health challenges in India requires a comprehensive approach that includes preventive, curative, and promotional strategies. By focusing on equitable access to quality healthcare, public health policies can create a healthier and more resilient population.
Reference:
- Public Health as a Problem-Solving Activity: Barriers to Effective Action - (https://www.ncbi.nlm.nih.gov/books/NBK218227/)
Source-Medindia