Phase 3 study demonstrates that neo-adjuvant chemoradiotherapy plus surgery, in esophageal or esophago-gastric-junction carcinoma, results in a higher survival rate than surgery treatment alone.
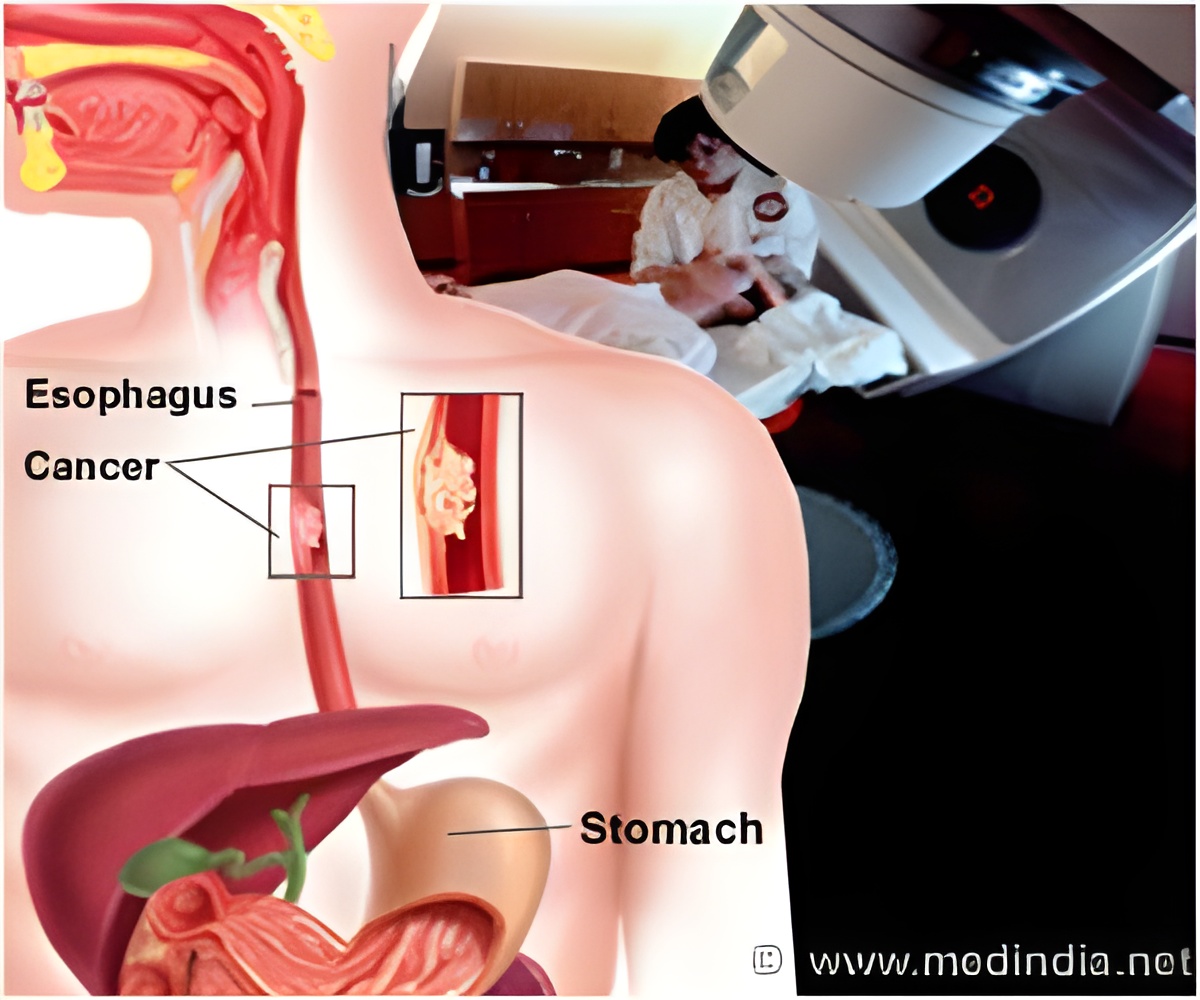
The trial enrolled patients aged 18 to 75 years, diagnosed with squamous-cell carcinoma, adenocarcinoma or large-cell undifferentiated carcinoma of the esophagus or esophagogastric junction i.e. the junction between the stomach and the esophagus. The cancers had not spread to distant organs. In addition, patients had ≤ 2 WHO performance status scores with ≤ 10% weight loss and no prior radiotherapy or chemotherapy experience.
Of the 368 enrolled patients, 188 patients with resectable tumors were randomly assigned to receive surgery alone while 178 patients received 5 weeks of carboplatin, paclitaxel and concurrent radiotherapy followed by surgery. Dexamethasone, clemastine, ranitidine and standard antiemetic agents were administered to all patients.
Surgery-only patients were operated soon after post-randomization Chemoradiotherapy patients underwent surgery within 4 to 6 weeks of chemoradiotherapy completion.
The table below provides the overall survival rates in the two treatment groups:
The pathological assessment revealed that complete tumor resection was attained in 92% patients in the chemoradiotherapy–surgery versus 69% patients in the surgery-only group. Complete pathological response was observed in 29% patients who underwent resection after chemoradiotherapy.
| Post-treatment years | Chemoradiotherapy-surgery patients | Surgery only group |
| 1 | 82% | 70% |
| 2 | 67% | 50% |
| 3 | 58% | 44% |
| 5 | 47% | 34% |
The pathological assessment revealed that complete tumor resection was attained in 92% patients in the chemoradiotherapy–surgery versus 69% patients in the surgery-only group. Complete pathological response was observed in 29% patients who underwent resection after chemoradiotherapy.
Thus, patients with cancers at the esophagus or the junction of the stomach and the esophagus experience a substantial increase in overall survival when treated before surgery with carboplatin-paclitaxel-radiotherapy combination.
Reference: Preoperative Chemoradiotherapy for Esophageal or Junctional Cancer; Van Hagen et al; N Engl J Med 2012; 366:2074-2084
Source-Medindia














