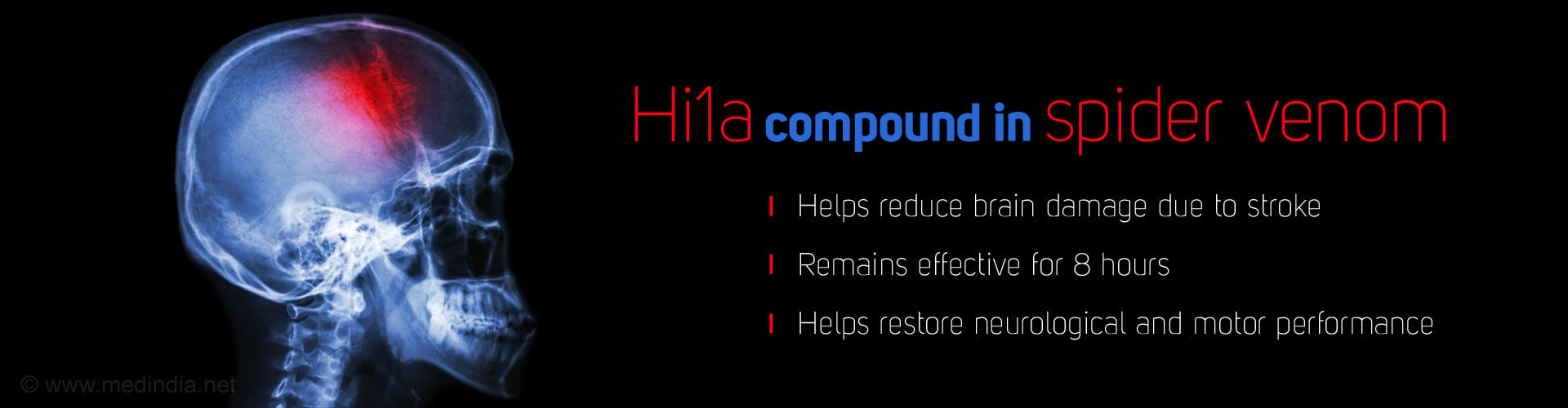
Venom from Darling Downs funnel web spider contains a molecule, Hi1a, which reduces the acid build up in the brain after a stroke and slows down brain damage.
Highlights
- The venom of one of the deadliest spiders in the world could be a source of drug to treat stroke.
- The molecule, called Hi1a, works by blocking ion channels in cells, specifically those that respond to the onset of acidic conditions in the brain.
- Clinical trials are yet to confirm the effect in humans.
Researchers discovered the protective molecule by chance as they sequenced the DNA of toxins in the venom of the Darling Downs funnel web spider (Hadronyche infensa) that lives in Queensland and New South Wales.
Venom from three spiders was gathered for the study after scientists trapped and “milked exhaustively” three spiders on Orchid beach.
The molecule, called Hi1a, stood out because it looked like two copies of another brain cell-protecting chemical stitched together. It was so intriguing that scientists decided to synthesise the compound and test its powers. “It proved to be even more potent,” said Glenn King at the University of Queensland’s centre for pain research.
In a series of studies on rats, King showed that a single small dose of the spider venom molecule protected neurons from induced strokes. The compound works by blocking what are called ion channels in cells, specifically those that respond to the onset of acidic conditions in the brain.
Rats that had the compound recovered far better than those that went without. “The untreated rats performed very badly after stroke. Their neurological and motor performance were terrible,” said King. But treatment with Hi1a “almost restored these functions to normal,” he added.
Approximately six million people a year die from stroke, making it the second largest cause of death worldwide after heart attacks. Strokes occur when blood flow to the brain is interrupted and the brain is starved of oxygen. About 85% of strokes are caused by blockages in blood vessels in the brain, with the rest due to bleeds when vessels rupture.
When a stroke happens, the oxygen level in the brain drops. This forces the brain to burn its primary fuel, glucose, very differently. Instead of oxidising glucose for energy, the brain switches to a process called anaerobic glycolysis. The reaction releases energy to keep the brain working, but it also produces acid, which can cause brain cells to die.
Clinical Trials Needed To Test the Compound
The researchers hope to start human trials of the compound in the next two years, but have more experiments to perform first. These will test whether the molecule works in all cases of stroke and is safe to use when blood vessels rupture in the brain, rather than become blocked.
In the latest study, the compound was infused directly into the brain, but the scientists have found since that nasal deliver works too. If trials show that the compound works, it could potentially transform the treatment of stroke patients. There are no drugs on the market that can protect the brain from stroke injuries.
The best hospitals can offer are infusions of clot-busting drugs if a clot is to blame, or a surgical procedure called endovascular thrombectomy, which physically pulls the clot from the brain. Before doctors can administer clot-busting drugs, they must confirm with a brain scan that the stroke was caused by a blockage. This is because the treatment thins the blood and could make matters worse if the stroke was caused by a haemorrhage.
If Hi1a is found to be safe for people who have had with brain bleeds, it could be given to patients as soon as they reach a doctor. “The drug could be given in the ambulance to most stroke patients before hospital arrival, maximising the number of neurons that can be saved,” said King. “This should diminish the mortality from stroke and provide much better outcomes for those that survive as more brain function will be retained.”
Kate Holmes at the Stroke Association, said it was unknown whether Hi1a could be an effective treatment in humans. “We welcome any treatment that has the potential to reduce the damage caused by stroke, particularly if this can benefit people who are unable to arrive at hospital quickly. Current treatments must be given in half this time period and it is too early for us to know if this research can offer an alternative for stroke patients,” she said.
Source-Medindia