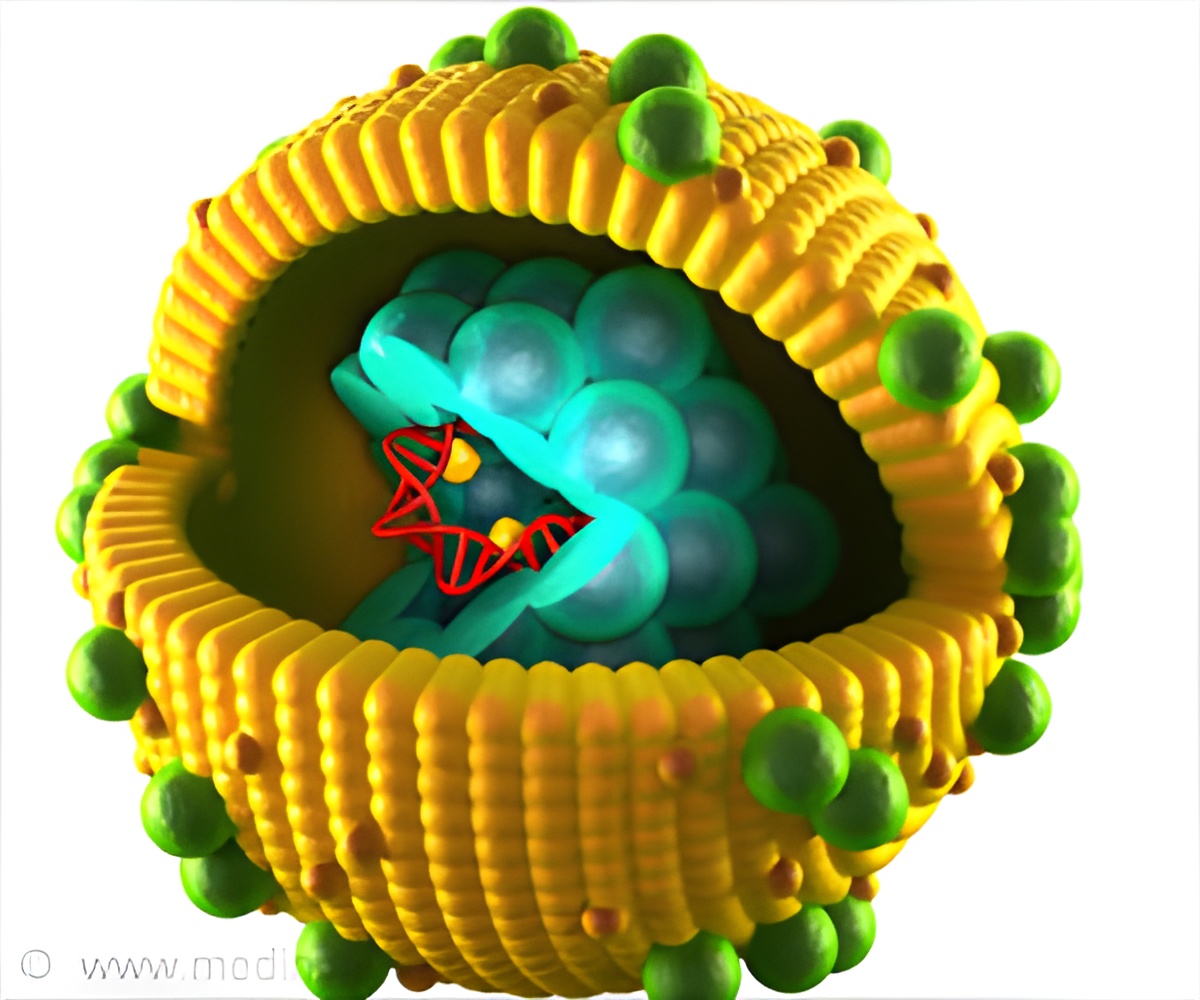
Chronic hepatitis B and C are life-threatening infectious diseases. Viral hepatitis has been neglected, resulting in ever increasing numbers of people dying from the disease.
‘Viral hepatitis elimination will require many interventions that are crucial for health system strength, as the emphasis is more on strengthening health systems.’





Despite the size of the challenge and the years of inaction, in 2016 WHO member states signed up to the goal of eliminating hepatitis B and C as a public health threat by 2030, now just 13 years away. This critical target was agreed because well evidenced solutions for the prevention and treatment of hepatitis B and C exist. Vaccination provides highly effective protection against hepatitis B, safe blood and infection control should be the basis of any health system, and harm reduction works. Existing treatment can effectively manage hepatitis B and prevent liver cancer, and new treatments can cure hepatitis C in nearly all patients.
However, efforts to address viral hepatitis are only just beginning. Few countries have established national plans that make treatment and prevention available for all patients. A lack of national and international investments in viral hepatitis programmes, especially in low-income and middle-income countries, mean that even fewer countries have a national plan that is properly funded. As a result, the vast majority of patients remain undiagnosed--91% of those with hepatitis B and 80% of those with hepatitis C--and only 1% are able to access treatment.
Even the birth dose hepatitis B vaccine, which can cost less than US$0·20, is not still used in many countries in Africa and the eastern Mediterranean region. Part of the problem is that hepatitis B and C are silent epidemics with few obvious symptoms for many years and often hit children and marginalised populations the hardest. Hepatitis B continues to spread unnoticed from mother to child at birth, putting infants at high risk: 80-90% of babies infected with hepatitis B will develop chronic disease and one in four will die of liver-related causes during adulthood.
Additionally, in low-income and middle-income countries, millions of people have been and continue to be infected, inadvertently and unnoticed, in health-care settings via the use of unsterilised equipment and unscreened blood transfusions. People living with HIV are also hard-hit by hepatitis B and hepatitis C, as are other stigmatised or marginalised groups with poor access to care, such as people who inject drugs, migrants, and indigenous populations. The commitment to eliminate hepatitis B and hepatitis C by 2030 matters because it offers the opportunity to prevent approximately 36 million infections and save 10 million lives.
Advertisement
Enhanced infection control services, including injection and blood safety and vaccination for health workers, will improve quality standards in health systems and reduce transmission of health-care-acquired illnesses for both patients and providers. Improved hepatitis B immunisation can help increase coverage of other childhood vaccinations and ensure that newborn babies receive appropriate postnatal care. Prevention of mother-to-child hepatitis B transmission can improve access to perinatal care, ensure healthy pregnancies, and promote institutional deliveries. Harm reduction efforts will help prevent the spread of blood-borne viruses such as HIV and syphilis.
Advertisement
Donors are needed to lay the groundwork for elimination in low-income and middle-income countries by supporting research and policy efforts to develop national hepatitis plans; providing financing and funding for the scale-up of cost-effective interventions; and supporting product and procurement investments to drive down drug and diagnostic prices and bring new technologies to market.
Hepatitis B and C can be eliminated but, given that in most countries the work is only just starting, there is not a moment to lose.
Source-Eurekalert