Risk of anemia in preterm infants with low birth weight revealed no improvement even after transfusion of higher threshold of hemoglobin.
‘Risk of anemia in preterm infants with low birth weight revealed no improvement even after transfusion of higher threshold of hemoglobin. This portrays that the transfusion threshold of hemoglobin increased the number of transfusions, but did not improve the chance of survival without neuro developmental impairment, among the babies at two years of age.’





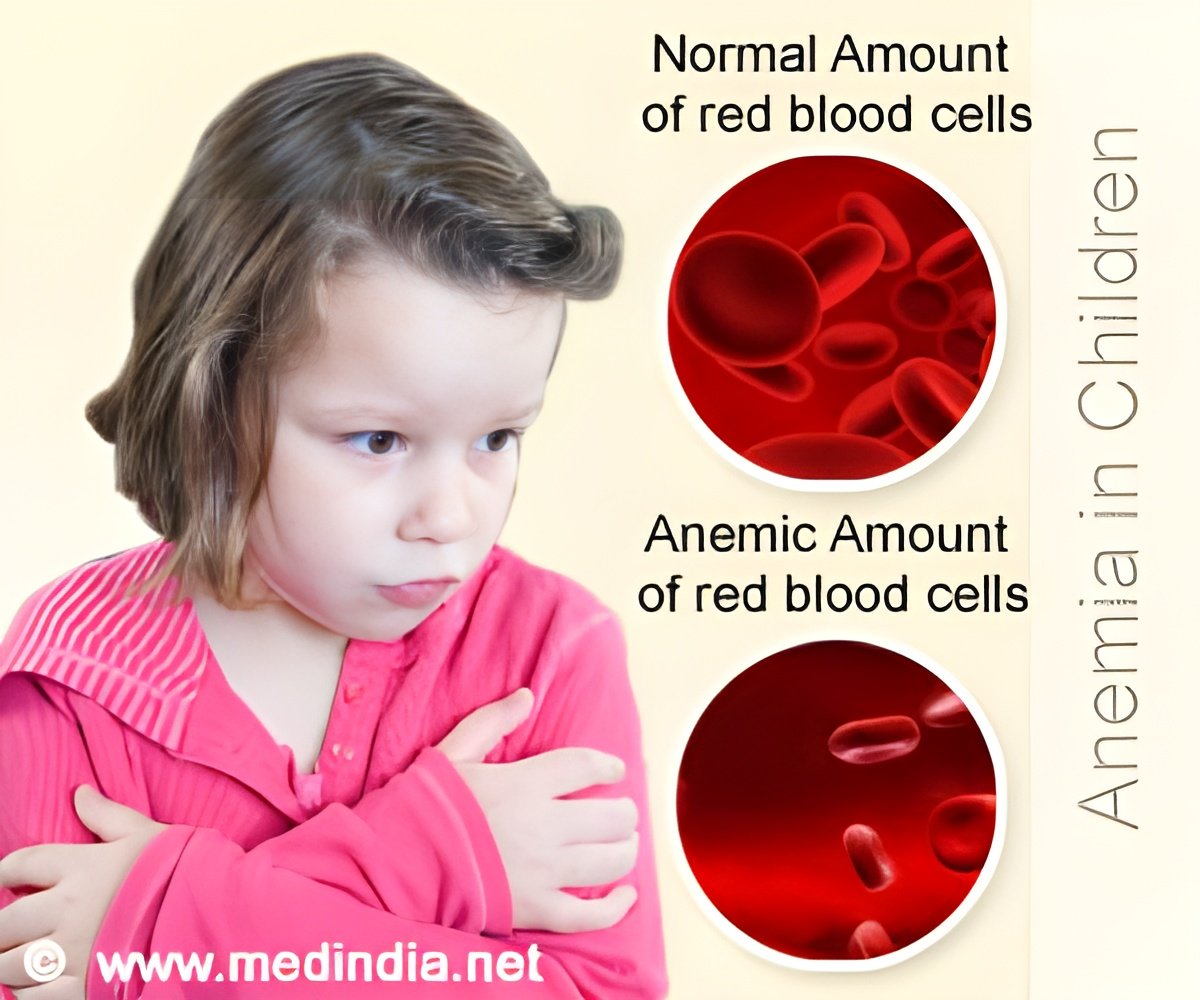
Preterm infants born before 29 weeks of pregnancy with weight less than 1,000 grams (slightly more than 2 pounds) are at high risk for anemia because of their early stage of development, reduced ability to produce red blood cells, and need for blood sampling as part of their intensive medical care. RBCs threshold in anemia
Previous studies suggest that anaemic infants who received transfusions at a higher hemoglobin threshold within the currently accepted range would have a lower risk of death or developmental problems. Measuring hemoglobin, a protein produced in red blood cells, indicates the proportion of red blood cells. Hemoglobin transfusion thresholds for preterm infants vary according to weight, stage of maturity and other factors.
845 infants were assigned to a higher hemoglobin threshold. Among them, 50.1% of them died or survived with neurodevelopmental impairment, as compared to 49.8% among 847 infants, who were assigned to a lower threshold.
When the two component outcomes were evaluated separately, the two groups also had similar rates of death (16.2% vs. 15%) and of neurodevelopmental impairment (39.6% vs 40.3%). It was observed that a higher hemoglobin threshold increased the number of transfusions, but did not improve the chance of survival without neuro developmental impairment, among the babies at two years of age.
Advertisement
Source-Medindia