Regular monitoring of lung function at home can be more effective for teens with Duchenne muscular dystrophy (DMD), reveals a new study.
‘Regular monitoring of lung function at home can be more effective for teens with Duchenne muscular dystrophy (DMD), reveals a new study. Home-based monitoring shows promise as an effective way to boost patient compliance while obtaining reliable clinical information without a hospital visit.’
Read More..




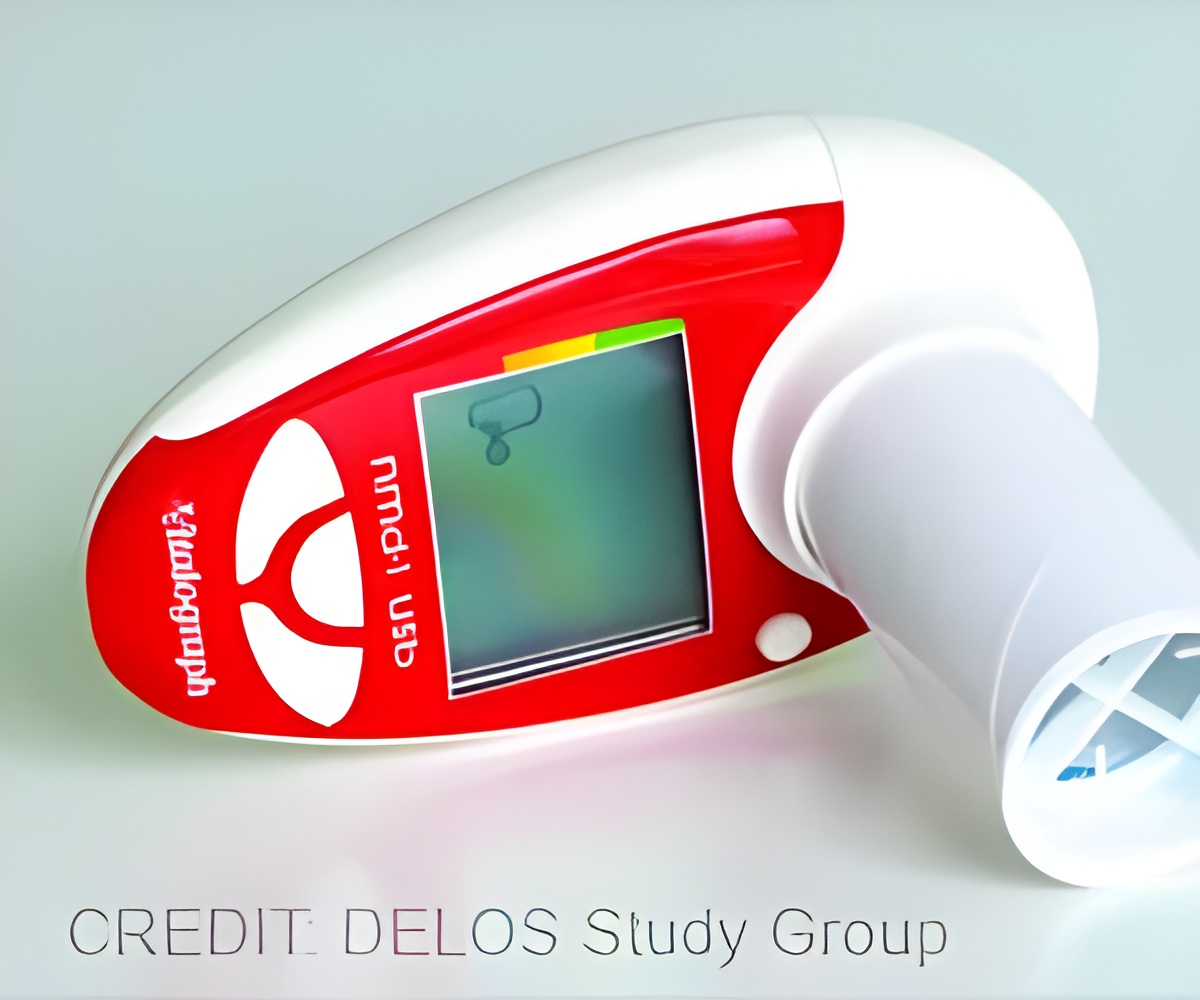
A new study describes the at-home use of a child-compatible, hand-held device (HHD) that makes monitoring pulmonary function in teens more convenient and provides the data needed for better disease management.Read More..
"This is the first study that demonstrates that the use of a hand-held device to assess pulmonary function is feasible in adolescent patients with DMD. Pulmonary function data obtained by this method are reliable as shown by comparison to standard spirometry results and participating patients showed a high level of adherence in the use of the device.
This new approach to collect pulmonary function data, together with several analyses methods, could be used in the planning of clinical intervention trials with respiratory function endpoints or to improve routine clinical care in patients with DMD," explained Prof. Gunnar M. Buyse, MD, PhD, Department of Paediatric Neurology, University Hospitals Leuven (Belgium).
DMD is a debilitating neuromuscular disease that is usually diagnosed in children between the ages of 3 and 5 years. During the early teenage years, patients with DMD find their mobility impaired and pulmonary function begins to deteriorate. Clinical symptoms include the inability to cough efficiently, poor airway clearance, recurrent respiratory infections and, eventually, respiratory failure necessitating ventilator support.
"Safeguarding pulmonary function, therefore, represents a significant unmet need," said Dr. Buyse.
Advertisement
The results showed that weekly use of the hand-held device was well accepted by adolescent trial participants over the course of a year, with average adherence exceeding 75 percent. Comparison of values for peak expiratory flow expressed as percent of predicted (PEF%p) collected with the hand-held device with data obtained on the same day with standard spirometry were highly correlated indicating the reliability of this method. Both assessment methods showed that idebenone treatment slowed the decline in pulmonary function compared to placebo.
Advertisement
Use of a hand-held device would offer an appropriate addition to hospital-based spirometry assessment with the advantage of allowing more frequent collection of pulmonary function data. Another possibility is that teenagers with limited mobility may be resistant to traveling to clinical centers.
Advantages of using home-based pulmonary function monitoring include the ability to obtain more frequent assessments, sometimes on a daily basis, which could facilitate early detection of pulmonary function decline. The study also showed that short observation periods (between 2 and 4 weeks) were sufficient to distinguish clinical changes in PEF%p. Finally, this method may prove to be very useful for the clinical testing of new therapies for DMD.
Source-Eurekalert