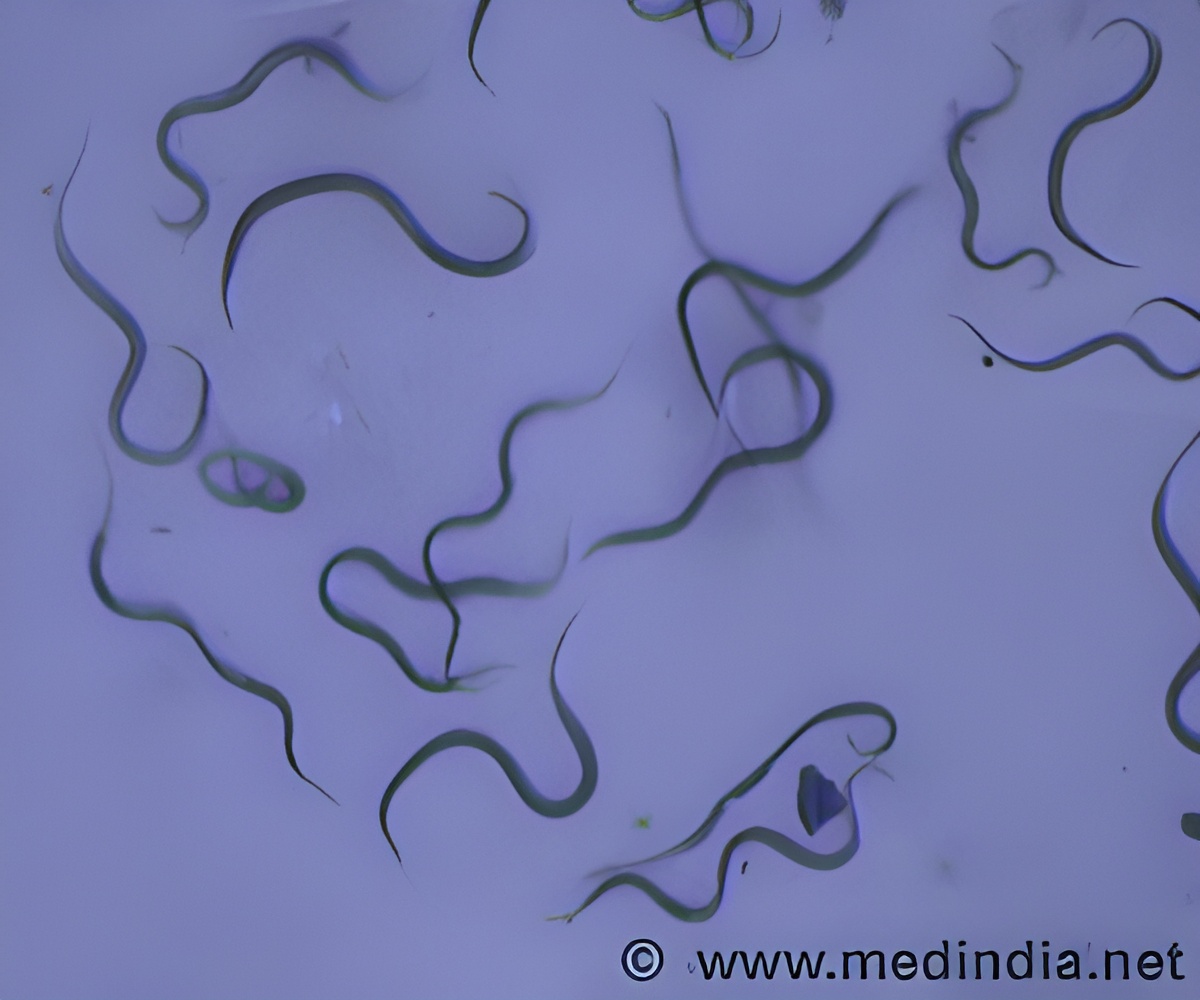
A new study has identified hospitals and long term care facilities as the hotbed for antibiotic-resistant Escherichia coli infections.
"The expansion of E. coli strain ST131 is recognized as a pandemic, but has received comparatively little attention in the United States," said Ritu Banerjee, lead investigator of the study. "Alarmingly, the pace of new antibiotic development has not kept up with the emergence of antibiotic-resistant E. coli, making development of strategies to halt further emergence and spread of these strains a public health priority."
In this retrospective study, investigators evaluated nearly 300 consecutive patients in Olmsted County, Minnesota with extraintestinal E. coli infections and found ST131 to be a dominant, antimicrobial-resistant clonal group associated with older age, long-term care facility residence, complicated infections, history of urinary tract infection, and prior antimicrobial use.
LTCF residence was the strongest predictor of ST131 infection, with LTCF residents having 8 times the risk of contracting E. coli ST131 compared with non-LTCF residents. This trend coincides with the increasing prevalence of ST131 among patients 65 years and older. It is likely that extensive antibiotic exposure, close contact with other antibiotic-exposed individuals, age and health-associated alterations in intestinal microbiota all contribute to the high prevalence of ST131 among the elderly population.
Patients with ST131 isolates were often treated with ineffective antibiotics at first and as a result they had recurrent or persistent symptoms. In the cohort, ST131 isolates were also more than twice as likely to be healthcare-associated infections as compared to community-associated infections.
"The finding that clonal expansion of ST131 is occurring primarily in healthcare and long-term care facilities indicates an urgent need for improved antibiotic use and infection control practices within such institutions, both to reduce selection for ST131 and to block further transmission. Efforts that focus on reducing overuse and misuse of fluoroquinolones are likely to have the greatest impact on ST131 prevalence, given the strong association between ST131 and fluoroquinolone resistance," said Banerjee.
Advertisement
Source-Eurekalert










