Atopic dermatitis affects the daily lives of nearly 20 percent of kids and up to 5 percent of adults. The condition can have a big impact on the quality of life of these patients.

‘Allergic skin diseases, such as atopic dermatitis, are clinically characterized by severe itching and type 2 immunity-related hypersensitivity to widely distributed allergens, including those derived from house dust mites.
’
Read More..




However, the mechanisms of hypersensitivity to allergens and immune system hyperactivity in patients with atopic dermatitis are not yet fully understood. Led by Inserm researcher Nicolas Gaudenzio, the young "IMMCEPTION" group studies the way in which the immune system interacts with sensory neurons to regulate inflammatory processes in atopic dermatitis.Read More..
In particular, the researchers have taken the lead from existing clinical data, which show that patients with this disease have numerous neuropeptides in their blood: chemical messengers that carry nerve messages, and whose level is correlated to disease severity.
The identification of these neuropeptides in the blood indicates the activation of the sensory neurons. These patients also have a number of enzymes in the blood, indicating the presence of mast cells. Mast cells are immune cells present in the skin that play an essential role in modulating inflammatory and allergic processes.
Based on these observations, Gaudenzio and his team decided to focus on the interaction between sensory neurons and mast cells, and have now published their findings in the scientific journal Nature Immunology.
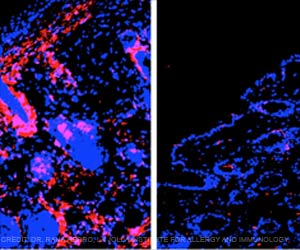
The researchers studied animal models of atopic dermatitis. Under the skin of mice showing signs of inflammatory reactions, they observed mast cells and sensory neurons clustering together in "sensory neuroimmune units" not dissimilar in form to a bunch of grapes. "The mast cells and neurons cling together in the dermis. We don't yet understand the molecular interactions that bind them together, but we have quantified the distances between them, which are tiny," highlights Gaudenzio.
Advertisement
In the longer term, this discovery could have practical therapeutic implications. "Until now, patients could be treated with biological treatments (biological therapy), but these obviously treat the disease further down the line, after flare-ups have occurred. We believe we have put our finger on a trigger mechanism and now want to continue our research to identify new molecules that could block interactions between mast cells and sensory neurons, and thus have a beneficial therapeutic effect for patients," explains the researcher.
"One of the questions we are now going to try and answer is what these mast cell-sensory neuron units are for. They must represent a defense mechanism for the body since they are also found in healthy individuals. But it could be that they don't work properly in people who have atopic dermatitis--that's what we're trying to understand," concludes Gaudenzio.
Source-Eurekalert