The discovery of T cells involvement in graft-versus-host disease is a vital step in finding more effective life-saving treatments for bone marrow transplant.
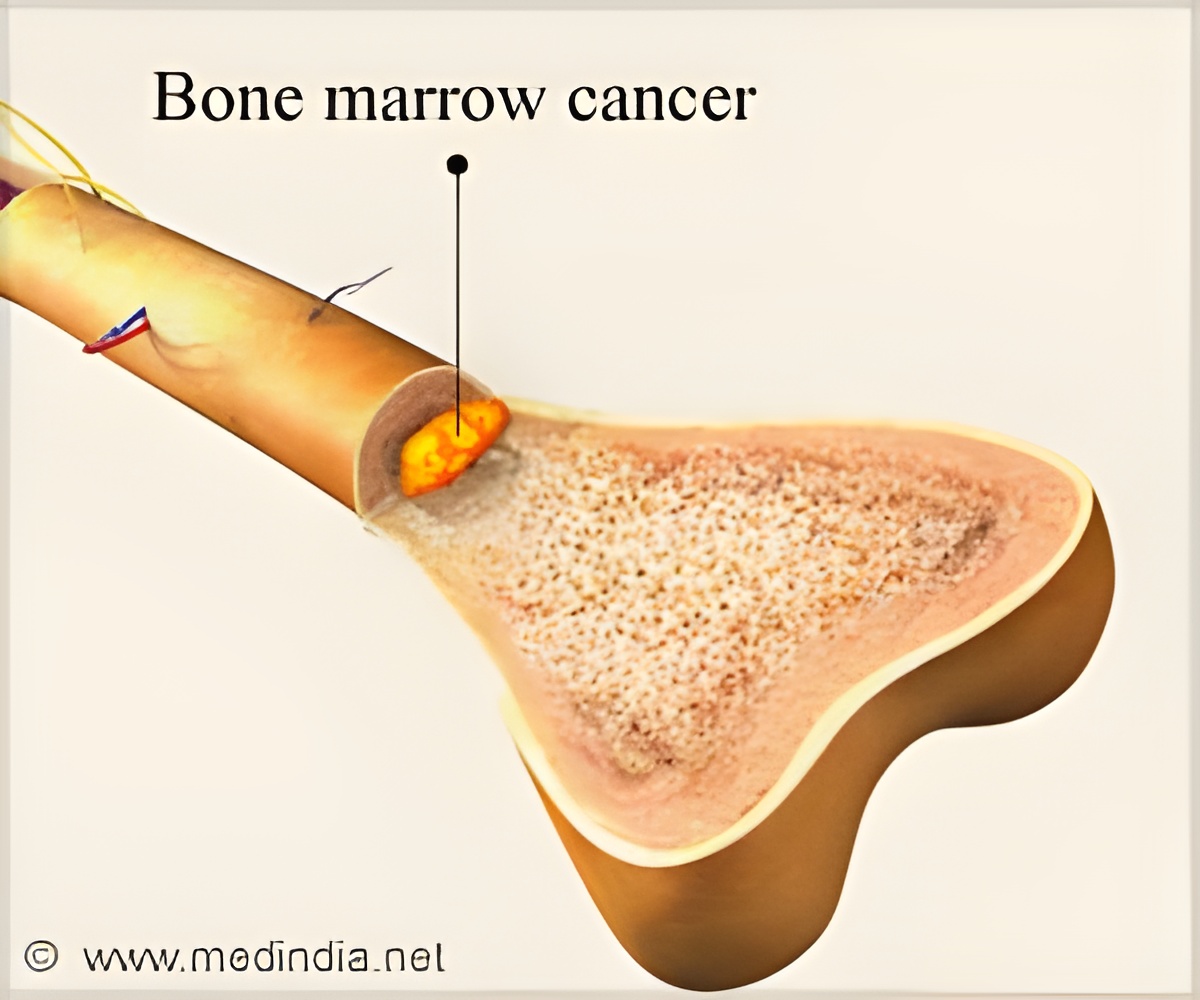
What is Graft Versus Host Disease
“Graft versus host disease is one of the most common complications after an allogeneic hematopoietic cell transplantation procedure, and the field knows quite well that the T cells from the donor are the ones mediating the disease,” says the study’s lead author Nicholas Hess, a scientist at UW–Madison’s Carbone Cancer Center. “Before this study, there was no finite T cell population that we've been able to identify as the cause of GVHD, so all our treatment regimens generally impacted the entire T cell population. But targeting all the T cells is not ideal, as they don't just cause this detrimental disease, they also have a beneficial impact on the ability to prevent relapses.”‘CD4/CD8 double positive T cells (DPT) that cause graft-versus-host disease is a key target that makes bone marrow transplants more effective. ’





“We looked at over 400 clinical samples from 35 patients as a part of this study and found double positive T cells to be predictive of GVHD. We also found four other biomarkers which are predictive of not just GVHD, but also relapse in general,” says Hess. “Based on that, our next step is to merge the biomarkers into a machine learning algorithm that can output a risk prediction model. Clinicians could then use this model to understand a patient’s risk of relapse and GVHD.” A team of physicians and scientists at UW–Madison is working on ways to address the problematic cells in patients while leaving healthy and helpful T cells to flourish.
“When we can gain confidence in this biomarker research and our ability to identify patients at risk, then we will potentially be able to treat them before they have all the detrimental effects of this disease,” Hess says.
The study won a Best Abstracts Award from the American Society for Transplantation and Cellular Therapy and was presented at the American Association of Immunologists (AAI) and ECOG-ACRIN conferences, creating excitement based on the findings’ potential impact beyond blood cancer and transplantation.
“I’ve learned that DPTs have been found in a variety of chronic human inflammatory diseases, which goes to show that this is not a specific thing to graft-versus-host disease. It's probably a wider phenomenon that these human T cells are doing that we've never really appreciated before,” says Hess. “It's very exciting because it gives us something to study further. I've always been interested in taking something you discover in the lab and translating it to the clinic. I think it's what gets me up every day. It is kind of the ultimate goal in my life to be able to say I participated in something that helped patients in some way.”
Advertisement