Link between statin use and the incidence of stroke risk in patients with atrial fibrillation has been explored.

What is Atrial Fibrillation
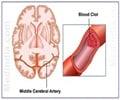
Atrial fibrillation is the most common heart rhythm disorder, affecting more than 40 million people worldwide. Patients with the condition have a five times greater risk of stroke than their peers. Anticoagulant medication is recommended to prevent strokes in those with atrial fibrillation but does not completely eliminate risk. Statin therapy is widely prescribed to lower blood cholesterol and reduce the likelihood of heart attack and stroke. However, the benefit of statins for stroke prevention in patients with atrial fibrillation has been unclear.‘New study supports the administration of statins to inhibit stroke and transient ischemic attack in atrial fibrillation patients.’





The researchers used the Hong Kong Clinical Data Analysis and Reporting System to identify all patients with a new diagnosis of atrial fibrillation between 2010 and 2018. Participants were divided into two groups: statin users and non-users. Users had received statins for at least 90 consecutive days during the year after being diagnosed with atrial fibrillation. The primary outcomes were the combined endpoint of ischemic stroke or systemic embolism; haemorrhagic stroke; and transient ischemic attack. Patients were followed until the occurrence of the primary outcomes, death or the end of the study on 31 October 2022.
Statins: The Key to Lower Stroke Risk in Patients
A total of 51,472 patients with a new diagnosis of atrial fibrillation were included, of which 11,866 were classified as statin users and 39,606 were non-users. The median age of participants was 75 years and 48% were women. During a median follow up of five years, statin users had a significantly lower risk of all primary outcomes compared to non-users. Statin use was associated with a 17% reduced risk of ischemic stroke or systemic embolism (hazard ratio [HR] 0.83; 95% confidence interval [CI] 0.78–0.89), a 7% reduced risk of hemorrhagic stroke (HR 0.93; 95% CI 0.89–0.98) and a 15% reduced risk of transient ischemic attack (HR 0.85; 95% CI 0.80–0.90).The researchers also found that long-term statin use was associated with greater protection than short-term use. Compared to those taking the medication for between three months and two years, patients using statins for six years or longer had a 43% lower risk of ischemic stroke or systemic embolism (HR 0.57; 95% CI 0.54–0.61), 44% reduced likelihood of hemorrhagic stroke (HR 0.56; 95% CI 0.53–0.60) and 42% reduced risk of transient ischemic attack (HR 0.58; 95% CI 0.52–0.64). These associations were consistent regardless of whether or not patients used anticoagulant medication and the type of anticoagulant.
The findings have important clinical implications particularly given that in atrial fibrillation patients, ischemic strokes are often fatal or disabling, and have a high risk of recurrence.”
Source-Eurekalert