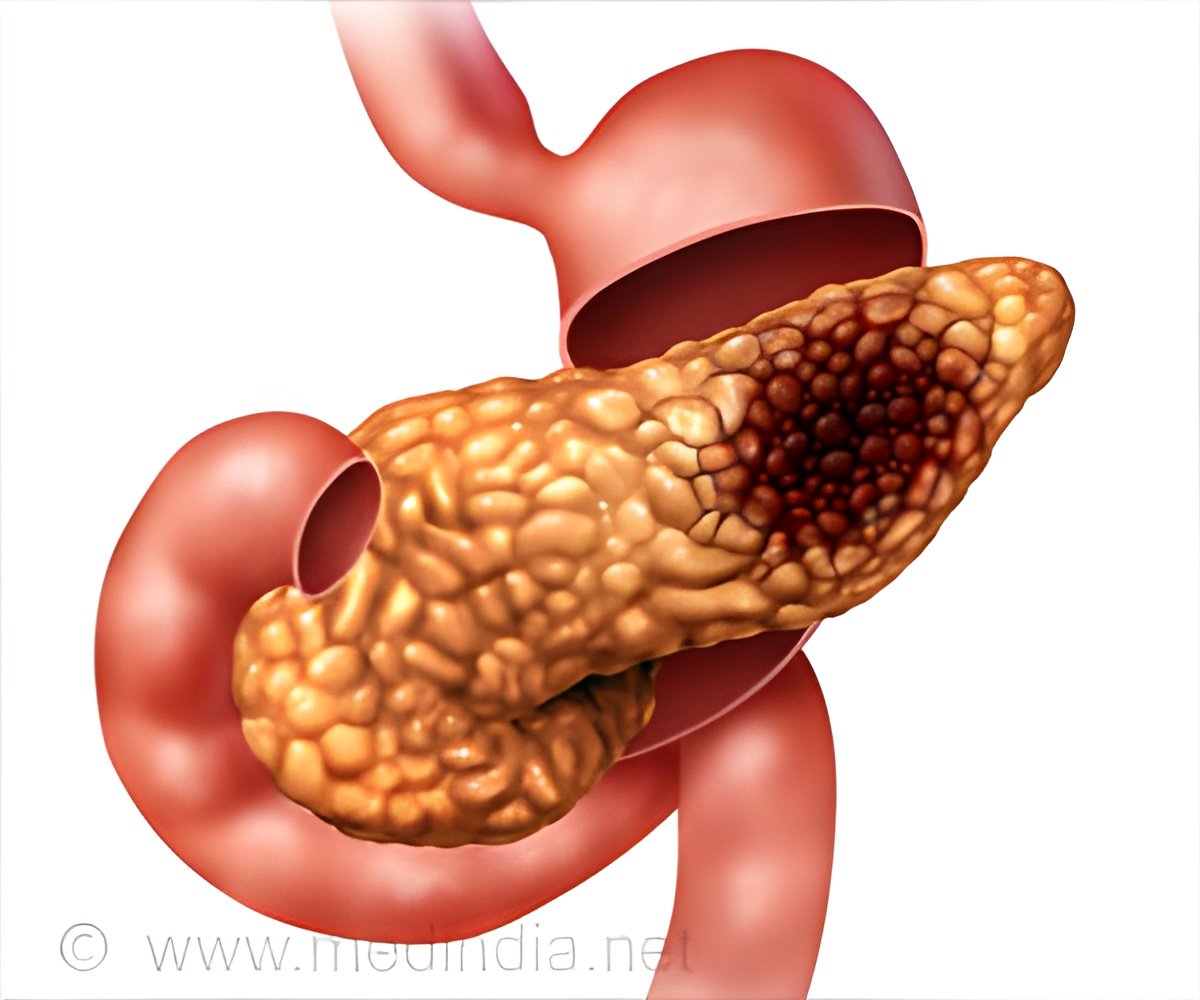
The comprehensive immune landscape and microbiome of pancreatic cysts outlined shows how they progress from benign cysts to pancreatic cancer.
Latest Findings on Pancreatic Cancer
Their findings, published in Lancet Gastroenterology and Hepatology, could reveal the mechanism of neoplastic progression and provide targets for immunotherapy to inhibit progression or treat invasive disease.‘The researchers also suggest that further studies addressing the tumor immune microenvironment of pre-invasive lesions are needed, including assessment of main-duct disease compared with branch-duct disease.’





"This will have far reaching implications on how we think about utilizing immunotherapies to treat certain types of pancreatic cancer, and also potentially inhibit the formation and progression of cancer from pancreatic cysts," said senior author Ajay V. Maker, MD, FACS, FSSO, a pancreatic surgeon, chief of UCSF’s division of surgical oncology, and Maurice Galante Distinguished professor of surgical oncology. The immune tumor microenvironment of the IPMNs evolves during malignant progression. A tumor microenvironment is the cellular environment that surrounds a tumor and includes immune cells and a stroma that supports other cells and tissues. A tumor and its microenvironment are constantly interacting with the microenvironment influencing both healthy and abnormal cell development (dysplasia).
As neoplasms progress from low-grade dysplasia to high-grade dysplasia and then to invasive carcinoma, a cytotoxic immune response rich in CD8+ T cells changes to an immunosuppressive environment with a measurable inflammatory response.
The researchers suggest that therapies that support cytotoxic T cells could be ideal for IPMNs with low-risk disease, whereas treatments that target regulatory T cells, myeloid-derived suppressor cells, and inhibitory macrophages could play a role in reducing malignant progression and treating high-risk disease. In addition to the treatment of IPMNs with an associated invasive carcinoma, addressing the immune tumor microenvironment could prevent the progression of IPMNs at high risk of malignant transformation.
The researchers discuss that with progressive amounts of dysplasia, the tumor microenvironment shows an increase in the concentration of pro-inflammatory and cyst fluid cytokines, which is indicative of a T-cell immunological response. The team’s research suggests that evaluation and characterization of the immune response to IPMNs could allow for early diagnosis, and potentially enhance treatments to halt progression or treat invasive disease.
Advertisement