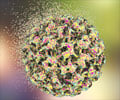
The human papillomavirus (HPV) vaccine known as Gardasil does not increase sexual activity among girls, finds study published in Pediatrics.

But the vaccine has been slow to catch on. By 2010, fewer than half of girls eligible for Gardasil had received even one dose. Since the introduction of Gardasil, there have been concerns—raised both in peer-reviewed literature and the popular media—that use of the vaccine might lead to increased sexual activity, due in part to the mistaken belief that Gardasil protects against pregnancy and sexually transmitted diseases other than HPV. This new study, which was an independent research project funded by Kaiser Permanente and Emory University, shows there is no evidence to support these concerns.
"Our study found a very similar rate of testing, diagnosis and counseling among girls who received the vaccine and girls who did not," said Robert Bednarczyk, PhD, an epidemiologist and the study's lead author. "We saw no increase in pregnancies, sexually transmitted infections or birth control counseling – all of which suggest the HPV vaccine does not have an impact on increased sexual activity."
Bednarczyk is a clinical investigator with the Kaiser Permanente Center for Health Research–Southeast in Atlanta, and an epidemiologist with the Rollins School of Public Health at Emory University.
"This is reassuring news for teenagers, parents, and members of the public. Our study adds to growing evidence that the HPV vaccine is a safe and effective way to prevent these rare but sometimes deadly cancers," added Robert Davis, MD, MPH, a co-author and senior investigator with the Kaiser Permanente Center for Health Research–Southeast.
The study included 1,398 girls ages 11 who were members of the Kaiser Permanente health plan in Georgia in 2006 and 2007, during the first 18 months after the Gardasil vaccine became available. Of this group, 493 girls received at least one dose of the HPV vaccine during the study period. The comparison group included 905 girls who received other recommended vaccines but not the HPV vaccine. Researchers followed both groups of girls for up to three years to assess whether they had been tested for or diagnosed with a sexually transmitted infection (STI), had taken a pregnancy test, and had been counseled about contraceptives.
About 10 percent of the girls in the study, both those who received the vaccine and those who did not, had one or more of these outcomes. The average age of testing, diagnosis, or counseling was about 14.5. Only eight girls, or less than 1 percent, were diagnosed with an STI or had a positive pregnancy test. Girls who received the HPV vaccine did not have a statistically higher rate of testing, diagnosis, or counseling compared to those who did not receive the vaccine.
This study is part of Kaiser Permanente's ongoing research to understand the safety and efficacy of Gardasil. In another study, published earlier this month in the Archives of Pediatric and Adolescent Medicine, Kaiser Permanente researchers confirmed the safety of the vaccine among nearly 200,000 young girls. Earlier this year in the Journal of Women's Health, Kaiser Permanente researchers reported that younger girls are more likely than women to report pain and other non-serious side effects after receiving Gardasil vaccine.
Source-Eurekalert