A new study reveals that two of the subtypes of human papillomavirus (HPV) that can be destroyed by vaccines were half as likely to be found in African American women compared to white women.

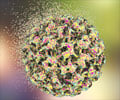
HPV is a common sexually transmitted infection with more than 40 subtypes. The virus causes nearly all cases of cervical cancer, which begin as precancerous cervical abnormalities. Two vaccines currently available to young women prevent infection by HPV 16 and HPV 18, the HPV strains responsible for about 70 percent cervical cancers.
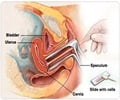
"Screening programs for cervical cancer are known to work well, with around 90 percent of sexually active women getting screened through Pap tests," said senior author Cathrine Hoyo, Ph.D., M.P.H., associate professor of obstetrics and gynecology at Duke University School of Medicine.
"The question is, if screening rates are comparable in African-American and white women, why are the rates of cervical cancer and mortality higher among African-American women when we have a program that works so well?"
Hoyo and her colleagues sought to better understand these disparities by determining if African-American and white women in the U.S. are infected with the same subtypes of HPV. The researchers enrolled 572 participants -- 280 African-American women and 292 non-Hispanic white women -- who came for additional testing after receiving abnormal Pap test results.
Of the 572 participants, 245 (43 percent) had no precancerous cervical abnormalities, 239 (42 percent) had early precancerous cervical abnormalities, and 88 (15 percent) had advanced precancerous cervical abnormalities. Seventy-three percent of the women infected with HPV were infected with multiple HPV subtypes.
Advertisement
In those with advanced precancerous cervical abnormalities, HPV 16, 18, 33, 39 and 59 were the most common genotypes detected in white women, whereas HPV 31, 35, 45, 56, 58, 66 and 68 were the most prevalent in African-American women.
Advertisement
A new HPV vaccine targeting nine HPV subtypes (6, 11, 16, 18, 31, 33, 45, 52 and 58) is currently being tested in phase III trials. While the new vaccine may help prevent additional HPV infections by covering new subtypes, it may not address the disparities found in this study.
"The most disconcerting part of this new vaccine is it doesn't include HPV 35, 66 and 68, three of the strains of HPV of which African-American women are getting the most," Hoyo said. "We may want to rethink how we develop these vaccines, given that African-Americans tend to be underrepresented in clinical trials."
The researchers noted that while these findings are compelling, the results are preliminary and the studies should be replicated in larger populations. Hoyo, Vidal and their colleagues are also continuing the research to define epigenetic marks that can be used to predict which precancerous cervical abnormalities will advance.
Source-Eurekalert