Hypothyroidism patients on levothyroxine feel worse and are much less active exhibiting cardiometabolic abnormalities despite having normal TSH levels.

‘Hypothyroidism patients who have lingering symptoms on levothyroxine might consult their physician about combination therapy that contains medications for both T3 and T4.’





Despite normal TSH tests, these patients still have many nagging symptoms of hypothyroidism. "Patients complain of being depressed, slow and having a foggy mind," said Rush's Antonio C. Bianco, MD, PhD, an immediate past president of the American Thyroid Association that is professor of medicine at Rush and an expert on thyroid disorders "They have difficulty losing weight. They complain of feeling sluggish and have less energy. Yet we doctors keep telling them, 'I'm giving you the right amount of medication and your TSH is normal. You should feel fine.'"New research gives these patients--who often feel dismissed and forgotten--evidence that their persistent symptoms are not just in their heads.
Research conducted by Bianco and other Rush colleagues published in the Journal of Clinical Endocrinology and Metabolism found that individuals on levothyroxine who had normal TSH levels were significantly more likely to be taking antidepressants than peers with normal thyroid function. The individuals taking thyroid medication were also less physically active, suggesting lower energy levels. They weighed about 10 pounds more than peers of the same height even though they consumed fewer calories, after adjustments for body weight. Plus, they were more likely to be using beta blockers, a drug frequently prescribed to lower blood pressure, and statins that reduce cholesterol levels.
"These findings correlate with what patients have been telling us," Bianco said. "This study documents for the first time, in an unbiased fashion, that patients on levothyroxine feel worse and are much less active than controls, exhibiting objective cardiometabolic abnormalities despite having normal TSH levels."
The Current Treatment Approach
Advertisement
One of the thyroid's primary jobs is to regulate metabolism, which affects almost every organ and function in the body. For example, when thyroid hormones are low, as in hypothyroidism, the heart rate slows and the intestines process food at a reduced speed, causing constipation. The thyroid also affects the brain. "Your brain turns off," Bianco said. "Patients are tired, sleepy and might experience feelings of depression. If not treated, might slow down dramatically and slowly go into a sleep state, and eventually into coma."
Advertisement
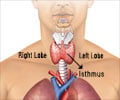
But things changed after scientists made two seminal discoveries. One is that the thyroid mostly produces T4, which turns into T3 as it travels through the body. "The important thing to understand is that T4 is not the active hormone," Bianco said. "T4 must be converted to T3 by our bodies with an enzyme called deiodinase."
This finding led to the widespread treatment of hypothyroidism with levothyroxine monotherapy, which is the pharmaceutical grade of T4. As Bianco explained: "The medical community reasoned, 'Hypothyroid patients should be given only T4 as opposed to giving desiccated thyroid with both T3 and T4. Then the body, in its wisdom, will make enough T3". This would avoid the potential side effects of giving straight active thyroid hormone T3.
The second discovery involved TSH, which is a hormone produced by the pituitary gland, a small organ at the base of the brain. Scientists determined that the pituitary and thyroid glands work together to ensure the body has enough T4 to turn into T3. When T4 levels are low as in hypothyroidism, the pituitary gland secretes TSH into the blood stream, stimulating the thyroid to produce more T4. A high TSH level in the blood is how physicians diagnose hypothyroidism, and they adjust up the dose of T4 (or the drug levothyroxine) until TSH levels are back in the normal range.
"That is how patients are generally treated and monitored today for hypothyroidism," Bianco said. "While the therapeutic goal is to make patients feel better, symptoms alone are not utilized for judging adequacy of treatment. Blood TSH levels are. In other words, the dose of levothyroxine is adjusted based on the TSH levels and not whether or not the patient feels better."
A Changing Paradigm
Because the majority of patients with hypothyroidism do well on levothyroxine monotherapy, which is considered a safe medication, the medical community has considered the treatment approach a success. However, in recent years, patient advocacy groups have helped draw attention to the plight of hypothyroid patients who feel sick despite taking levothyroxine and having normal TSH levels.
Because he and his colleagues specialize in thyroid disorders, Bianco tends to see a lot of these patients. "What they're looking for is someone to believe what they're saying," he said. "When I say, 'I understand and I believe you,' many of my patients start crying. These patients have been suffering and physicians have been dismissing them."
To learn more about why some patients were not feeling well in a completely objective, unbiased fashion, Rush researchers turned to a large publicly available survey, called the U.S. National Health and Nutrition Examination Survey (NHANES). More than 10,000 people participate in NHANES, a program of studies designed to assess the health and nutritional status of adults and children in the United States. The survey is unique in that it combines interviews and physical examinations.
From that database, the Rush researchers identified 469 adults who were taking levothyroxine monotherapy and compared them to 469 individuals who were not on levothyroxine. Both groups were matched for age, sex, race, and serum TSH levels.
"We looked to see how 52 clinical measures differed between the two groups. Individuals taking levothyroxine weighed significantly more and moved less, they were also more likely to take antidepressants than those who were in the control group," said Sarah Peterson, PhD, first author of the study and registered dietitian at Rush University Medical Center.
Other findings included a significantly higher use of statins and beta blockers in the levothyroxine group, presumably for high cholesterol and high blood pressure.
A Revised Dialogue
Hypothyroid patients who continue to have symptoms on levothyroxine monotherapy might talk to their physician about trying combination therapy, or a pill that contains both T3 and T4. Trials of combination therapy are supported by the American Thyroid Association, but clinical studies are mixed on whether this approach works, Bianco said. Subjectively, some patients report feeling better and others don't.
Better medications are needed to treat hypothyroidism, Bianco believes. Until that day, he urges physicians to change how they talk about hypothyroidism treatment with patients. "Doctors should be telling their patients, 'I'm going to normalize your TSH, but you're going to be at a higher risk for gaining weight, experiencing depression and fatigue. It is also more likely that your cholesterol will go up.' That's what we should be telling patients, based on our study. This conversation is particularly important for any patient that is considering surgical removal of the thyroid gland".
Source-Eurekalert