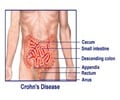
Discover the role of biomarkers in diagnosing and managing Inflammatory Bowel Disease (IBD), including Crohn's Disease and Ulcerative Colitis.

‘#Inflammatory_Bowel_Disease (IBD) affects approximately one in 200 people in developed countries and its prevalence increasing in underdeveloped and newly industrialized regions. #crohndisease #ulcerativecolitis #biomarkers #medindia
’





Inflammatory Bowel Disease (IBD) is quite common, affecting one in 200 people in developed countries and on the rise in underdeveloped and newly industrialized countries, which puts a significant strain on healthcare systems. Effectively managing inflammatory bowel disease (IBD) is still difficult because of the vague nature of its clinical presentations and the absence of a gold-standard diagnostic test.
As a result, accurate and widely available biomarkers for monitoring disease activity and predicting therapy response are critical. This review provides a thorough analysis of the state of biomarkers used in IBD management.
By highlighting the applications, threshold values, and clinical concerns of both known and new biomarkers, the writers examine them all. The study was published in the Journal of Translational Gastroenterology(1✔ ✔Trusted Source
Use of Biomarkers in the Management of Inflammatory Bowel Disease
Go to source).
Biomarkers in Inflammatory Bowel Disease Diagnosis
C-reactive protein
(CRP) is one of the most widely used biomarkers for monitoring IBD activity due to its low cost, ease of testing, and well-established protocols. It is an acute-phase reactant produced by hepatocytes in response to pro-inflammatory cytokines.Advertisement
CRP is particularly useful in CD, where it correlates with moderate to severe clinical activity and evidence of active disease on ileocolonoscopy.
Advertisement
Erythrocyte sedimentation rate
(ESR) is another commonly tested marker of inflammation, though it lacks specificity similar to CRP. It differs from CRP in its slower response to inflammation and longer normalization time.ESR can be affected by physiological factors such as pregnancy, age, and gender, as well as medication use, highlighting the importance of interpreting results in context.
Vitamin D
deficiency is prevalent in IBD patients and is associated with an increased risk of disease recurrence, hospitalizations, and surgeries.Its role as an immune modulator suggests therapeutic potential, though further research is needed to determine optimal supplementation levels and therapeutic benefits.
Platelets
often overlooked in IBD evaluations, play an active role in inflammatory processes.Reactive thrombocytosis, a well-established phenomenon in inflammation, has been observed in IBD patients, with platelets exhibiting an increased sensitivity to activation even in clinically silent diseases. Platelet changes may correlate with disease relapse in UC.
Novel Biomarkers for Inflammatory Bowel Disease Diagnosis
Recent studies have focused on developing novel biomarkers with improved specificity and predictive value for IBD management. Examples include:Mucosal addressin cell-adhesion molecule-1 (MAdCAM-1)
Elevated levels of MAdCAM-1 have been associated with inflammation and may predict response to vedolizumab, a monoclonal antibody used in IBD treatment.Oncostatin M
Elevated oncostatin M levels could predict the risk of IBD development and potentially nonresponse to vedolizumab or corticosteroids.NOD2 mutations
Genetic analysis for NOD2 mutations may be predictive of fibrostenotic disease in CD, though it is not specific for treatment response.Anti-Integrin αvβ6
Blood levels of anti-Integrin αvβ6 are useful for diagnosing and predicting disease severity in UC, though they do not specifically predict treatment response.In conclusion, biomarkers play a crucial role in managing IBD. While established markers like CRP, ESR, vitamin D, and platelets remain essential, novel biomarkers hold promise for improving diagnostic accuracy and predicting treatment response.
Future research should focus on developing more sensitive and specific biomarkers to guide personalized treatment, potentially using combined biomarker panels for more effective IBD management.
Reference:
- Use of Biomarkers in the Management of Inflammatory Bowel Disease- (https:www.xiahepublishing.com/2994-8754/JTG-2023-00086)
Source-Eurekalert