According to research, the lot-busting drug tenecteplase prevents death or circulatory collapse appears to be especially useful in patients younger than 75.
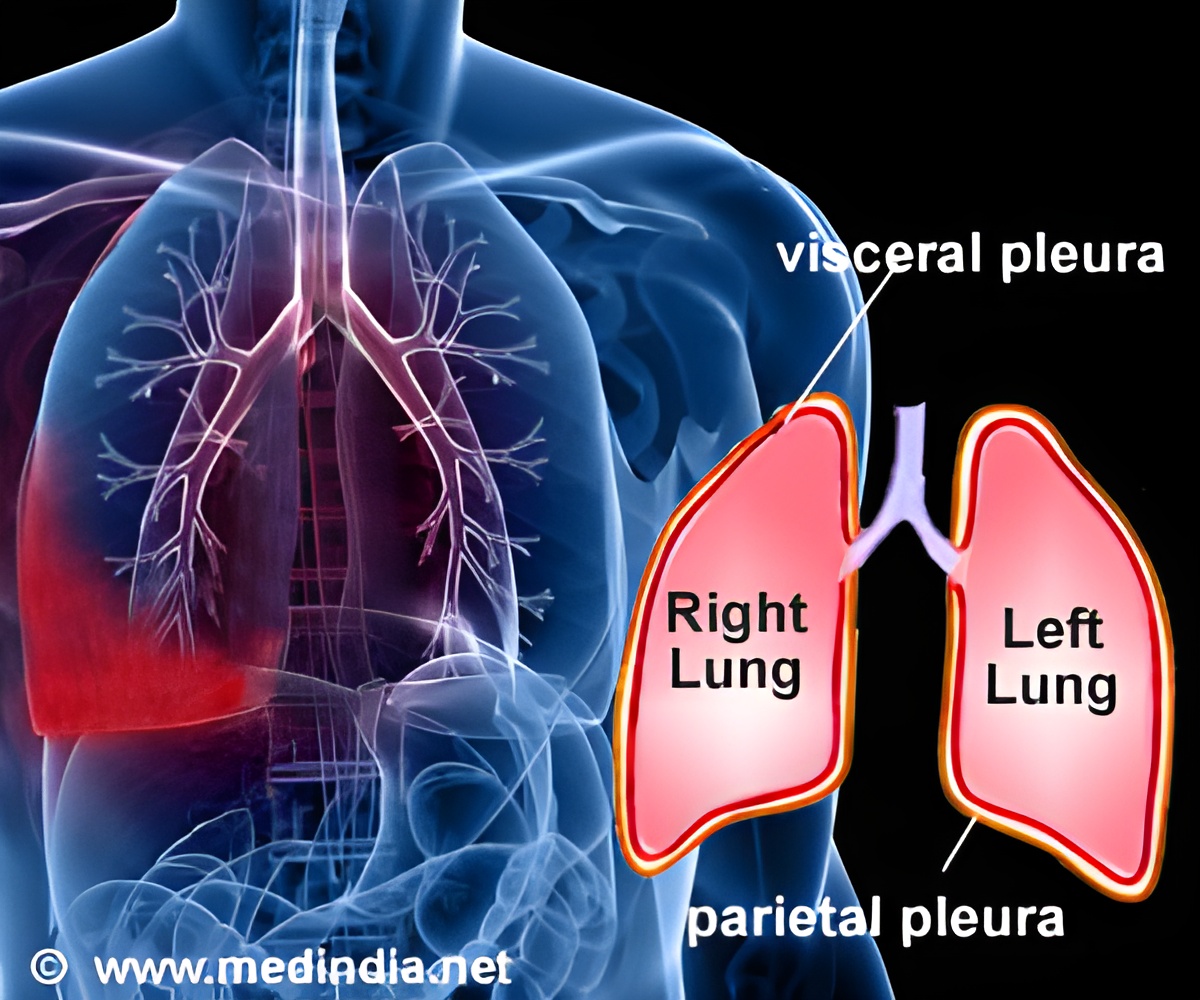
Heparin is the current standard therapy for most patients, including a subgroup of patients that is said to have submassive or intermediate-risk pulmonary embolism: that is, they have normal blood pressure but dysfunction of the heart's right ventricle, which can be seen on an echocardiogram or CT scan. Blood tests also can help to identify these patients.
The Pulmonary Embolism Thrombolysis Study (PEITHO) tested the addition of a clot-busting (thrombolytic) drug, tenecteplase, to standard treatment with heparin. Tenecteplase dissolves blood clots rapidly but carries a known risk of bleeding in the brain. The double-blind study included 1,006 patients in 13 countries. They were randomized to heparin plus placebo or heparin plus tenecteplase.
The combined primary endpoint was death from any cause or circulatory system (hemodynamic) collapse after seven days. Hemodynamic collapse was defined as at least one of the following: needing CPR due to a loss of blood pressure; systolic blood pressure of less than 90 mm Hg or a drop of more than 40 mm Hg for at least 15 minutes; or the need for drugs called catecholamines, which boost circulation.
The primary endpoint was reduced by 56 percent in patients treated with tenecteplase and heparin, compared with the heparin-only group.
"In patients with intermediate-risk pulmonary embolism, thrombolytic treatment significantly reduced the primary endpoint," said Stavros Konstantinides, MD, PhD, professor for clinical trials at the Center for Thrombosis and Hemostasis, University of Mainz, Germany, and the study's co-principal investigator. "Overall, the study strongly supports the concept that risk stratification of patients makes sense and that these patients need something to prevent deterioration."
Advertisement
Major bleeding was significantly increased with tenecteplase: 6.3 vs. 1.5 percent in the placebo group.There were 10 hemorrhagic strokes in the tenecteplase group and one in the placebo group.
Advertisement
Source-Eurekalert