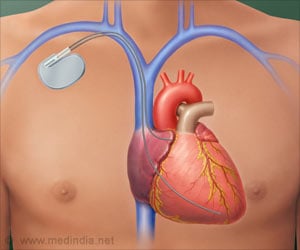
Researchers uncovered an association between heart disease and chronic kidney disease.
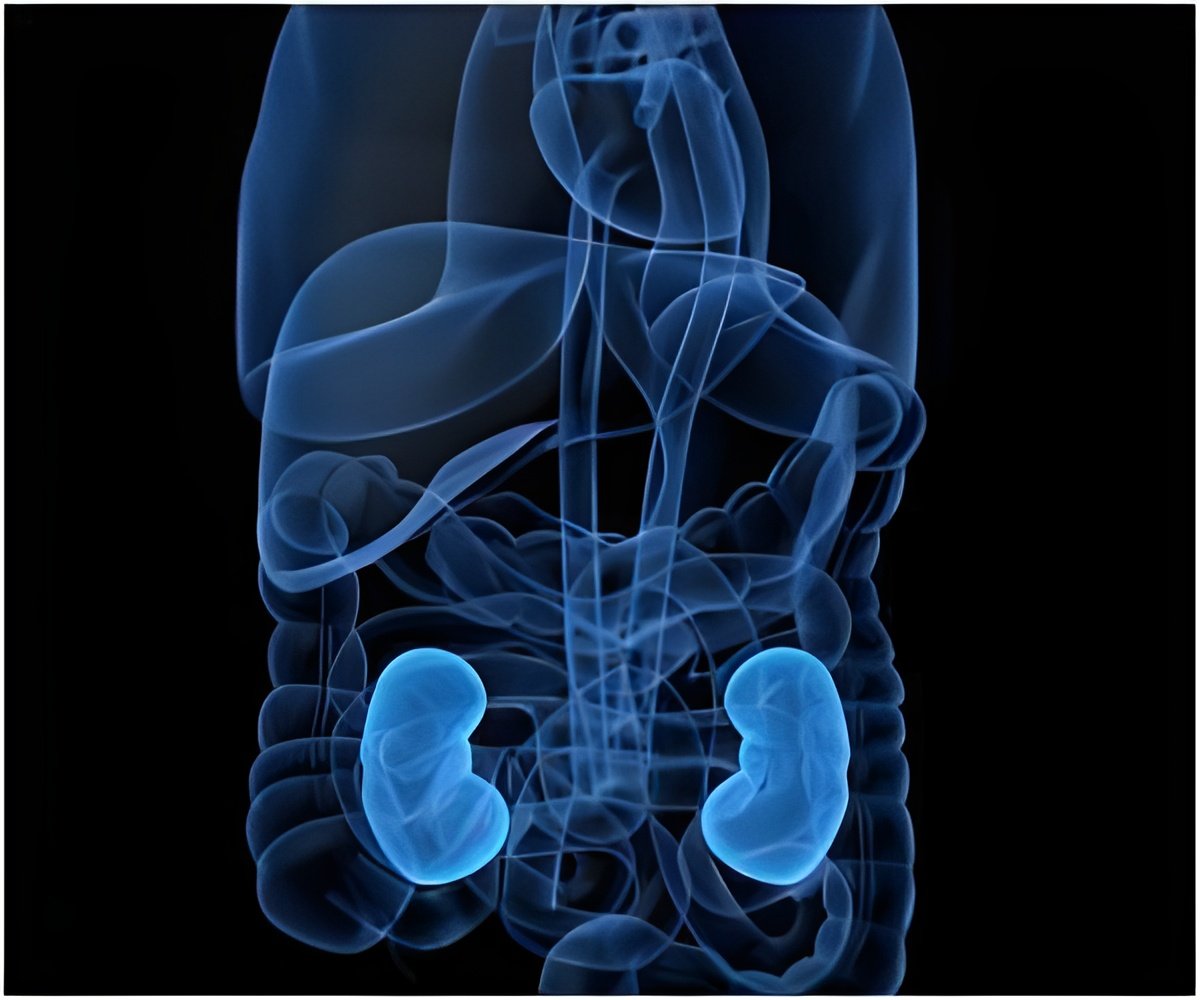
A Closer Look at Chronic Kidney Disease and Cardiovascular Disease
sEVs are naturally secreted by all cells. They carry and spread a variety of signaling molecules between cells, including proteins, microRNA (miRNA), and DNA. The team sequenced the population of miRNAs in circulating sEVs and found that four miRNAs were decreased in sEVs from both a rodent model and from humans with chronic kidney disease. These miRNAs are protective against vascular calcification. “Computational analysis showed that this quartet of miRNAs targets VEGFA–VEGFR2 signaling, which is a key signaling pathway that drives vascular calcification,” explains joint first author Takaaki Koide. “The reduction in the miRNA levels was linked to an increased amount of VEGFA protein”.‘Small extracellular vesicles (sEVs) initiating from chronic kidney disease play key role in blood vessel calcification which causes heart disease. ’





“We then showed that therapeutic inhibition of the VEGFA pathway, both pharmacologically and genetically, reduced the vascular calcification in our rodent model of chronic kidney disease,” explains Shintaro Mandai, joint first author. Treatment of chronic kidney disease patients with these VEGFA inhibitors may potentially lessen the associated vascular calcification. Targeting the sEVs themselves may also have therapeutic potential. “The quartet of miRNAs also showed diagnostic efficiency, as the expression level of each miRNA is useful for predicting calcification of the abdominal aorta,” explains senior author Shinichi Uchida. “These miRNAs are therefore strong candidates as both biomarkers of disease and therapeutic targets.”
This study reveals for the first time that vascular calcification is controlled by VEGFA signaling that is activated by sEVs derived from chronic kidney disease. It could prove key to the treatment of these diseases, which are highly significant worldwide.
Source-Eurekalert