Current guidance from multiple professional organizations recommend vaccination for all eligible organ transplant recipients. But more studies are needed to characterize the safety, immunogenicity, and ultimately, efficacy of SARS-CoV-2 vaccines for transplant recipients.

‘As immunosuppression may increase SARS-CoV-2 viral load and prolong the duration of SARS-CoV-2 viral shedding and transmissibility, studies to monitor both symptomatic and asymptomatic infection should be done.’
Read More..




The majority of viral-vectored vaccines in the most advanced phases of development have been rendered replication-deficient through deletion of genes essential for replication. By limiting vector replication, the potential for vaccine-associated AdV disease is greatly diminished.Read More..
There are, however, theoretical mechanisms by which replication-deficient viral vector–based vaccines could become replication competent and cause disease, especially in immunocompromised individuals.
Though infrequent, severe AdV infections, including allograft nephritis, can occur in kidney transplant recipients during natural infection.
Vaccine-associated AdV disease has not been reported, albeit there is little experience in immunocompromised populations.
Despite the theoretical concerns with replication-deficient viral vector–based vaccines, immunosuppression is not considered a contraindication to their use.
Advertisement
Other vaccine candidates that are in advanced stages of development, including mRNA, protein subunit, or whole virus–inactivated SARS-CoV-2 vaccines, do not contain intact virus and thus do not carry a risk of vaccine-associated infection.
Advertisement
Acute allograft rejection is uncommon during COVID-19, despite frequent reduction in immunosuppression as a therapeutic strategy.
In the absence of an observed association between natural SARS-CoV-2 infection and acute allograft rejection in kidney transplant recipients, it is unlikely that vaccine antigens would precipitate clinically significant immune responses to renal allografts.
In general, adjuvants used to enhance vaccine immunogenicity also elicit nonspecific inflammatory responses, and thus have the potential to induce acute allograft rejection.
Concern about adjuvant safety in organ transplant recipients arose from observations of an unusually high incidence of anti-HLA antibodies in kidney transplant recipients who received the 2009 influenza A(H1Na1)pdm09 vaccine, which contained the squalene-based AS03 adjuvant system.
However, only a fraction of these anti-HLA antibodies were donor specific, and a subsequent investigation of >10,000 solid organ transplant recipients found no definitive association between the AS03 adjuvant system and acute allograft rejection.
Several recombinant spike protein SARS-CoV-2 vaccines contain adjuvants, such as AS03 and the novel Matrix M1 adjuvant, which contains the same QS21 saponin found in the recombinant varicella zoster vaccine.
Viral-vectored and mRNA vaccines do not generally contain adjuvants, although lipid nanoparticle delivery devices used in the mRNA vaccines have natural adjuvant activity.
Postmarketing surveillance will be essential to assess any potential association between SARS-CoV-2 vaccine components and acute allograft rejection.
In the interim, theoretical concerns associated with any vaccine must be weighed against the benefits of preventing or mitigating the severity of a life-threatening infection in a vulnerable population.
We emphasize that a broad range of vaccines have a substantial track record of safety in kidney and other solid organ transplant recipients. Furthermore, no definitive association between any vaccine or adjuvant and allograft rejection has been identified to date.
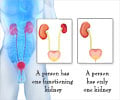
Immunosuppression in kidney transplant recipients is anticipated to reduce the immunogenicity of SARS-CoV-2 vaccines, and immunogenicity may vary by vaccine platform.
Available data suggest they have relative humoral response rates that are approximately 50%–70% of those seen in nontransplant populations.
Patients with ESRD may have more a robust response to vaccines before rather than after kidney transplant,6 and when possible, SARS-CoV-2 vaccines should be given before transplantation.
In the post-transplant setting, age >65 years, more recent transplantation, use of mycophenolate and mammalian target of rapamycin inhibitors, and lower graft function are associated with decreased serologic responses to influenza vaccines.
Despite the effects of lymphocyte-depleting immunosuppression in the early period after transplant or treatment for rejection, the benefits of even modest SARS-CoV-2 protection might outweigh the risk of delaying immunization during a pandemic.
In general, vaccines are not recommended immediately post-transplant due to a presumed decrease in immunogenicity after recent high-level immunosuppression.
Expert opinion advises that delaying SARS-CoV-2 vaccination of vaccine-naive transplant recipients until 3 months after transplant or receipt of T cell or B cell ablative therapies may be appropriate; for patients who received a first dose before transplant, administration of the second dose should be delayed until at least 4 weeks post-transplant.
Higher doses, booster doses, adjuvants, and intradermal delivery have all been used with variable success to improve immunogenicity of commonly administered vaccines in solid organ transplant recipients.
If immunogenicity of standard regimens in kidney transplant recipients is suboptimal, these alternative approaches should be considered.
The diversity of vaccine platforms and phased vaccine allocation present unique challenges for assessing the safety, immunogenicity, and efficacy of SARS-CoV-2 vaccination in kidney transplant recipients.
Surveillance for adverse events related to each specific formulation through prospective multicenter registries of vaccinated solid organ transplant recipients is one potential approach to assessing safety, especially given that large population-specific studies of kidney transplant recipients may not be feasible.
Prospective clinical trials should directly compare different SARS-CoV-2 vaccine platforms, assess the magnitude and durability of humoral and cellular responses, and utilize the same functional laboratory immunogenicity assays as the vaccine trials to facilitate direct comparisons between transplant recipients and general populations.
Future investigations may identify relevant differences among the various vaccine platforms to guide future studies of alternative vaccination strategies, if warranted.
Because transplant recipients’ responses to vaccines may be suboptimal, continued emphasis should be laid on nonvaccine preventive measures.
Vaccination of caregivers and close contacts of kidney transplant recipients, recommended for influenza vaccination, would be an important strategy to reduce the risk of infection.
Assessment of vaccine efficacy against emerging SARS-CoV-2 variants is vital to establish optimal vaccine strategies for both immunocompetent and immunocompromised populations.
SARS-CoV-2 vaccines may add to the armamentarium of vaccines that have safely protected transplant recipients from serious infectious diseases for decades.
Source-Medindia