The analysis of data from two Swedish registries was presented by Dr Anders Ulvenstam, and shows that the reduction is due to improvements in AMI care.
"The risk of ischemic stroke after myocardial infarction has been studied previously, but there are many questions that remain unanswered," said Dr Ulvenstam. "Many studies have been conducted within clinical trials but these trials tend to focus on a particular patient group. Few, if any, studies have been done on the broader group of patients seen in day to day clinical practice. We based our analysis on two registries which include all AMI patients in Sweden."
"Great variation in the incidence of ischemic stroke after AMI has been found in previous studies, which tells us that we do not have a realistic estimate of the risk of suffering from ischemic stroke after myocardial infarction," he added. "Furthermore, many of the earlier studies were done before modern AMI care -with different drugs and interventional procedures- was established, which is why we do not know how this has affected the risk over time. There is also conflicting data regarding independent predictors of stroke risk."
The study presented at ESC Congress 2012 was based on 173,233 Swedish AMI patients between 1998-2008, from the Register of Information and Knowledge about Swedish Heart Intensive Care Admissions (RIKS-HIA). In order to identify which of these AMI patients suffered an ischemic stroke within one year, the RIKS-HIA database was merged with the Swedish National Registry, which contains diagnoses for all patients at discharge from hospital care.
Dr Ulvenstam said: "Based on this patient information we were able to answer the questions raised above, regarding the incidence, time trends and independent predictors of ischemic stroke at one year after AMI."
The researchers found that during 1998-2008 the average risk of ischemic stroke one year after AMI was 4.1%. This was nearly twice as high as the incidence found in an important meta-analysis performed by Witt et al. in 2006 which showed an average risk of 2.1% (1). Dr Ulvenstam said: "The higher incidence in our study could be explained by the fact that we have such an unselected patient group. The registries used exclude very few AMI patients which means that there are more potential stroke victims."
Advertisement
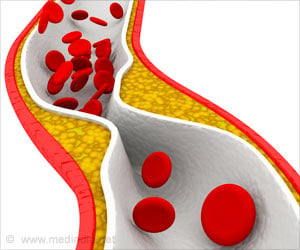
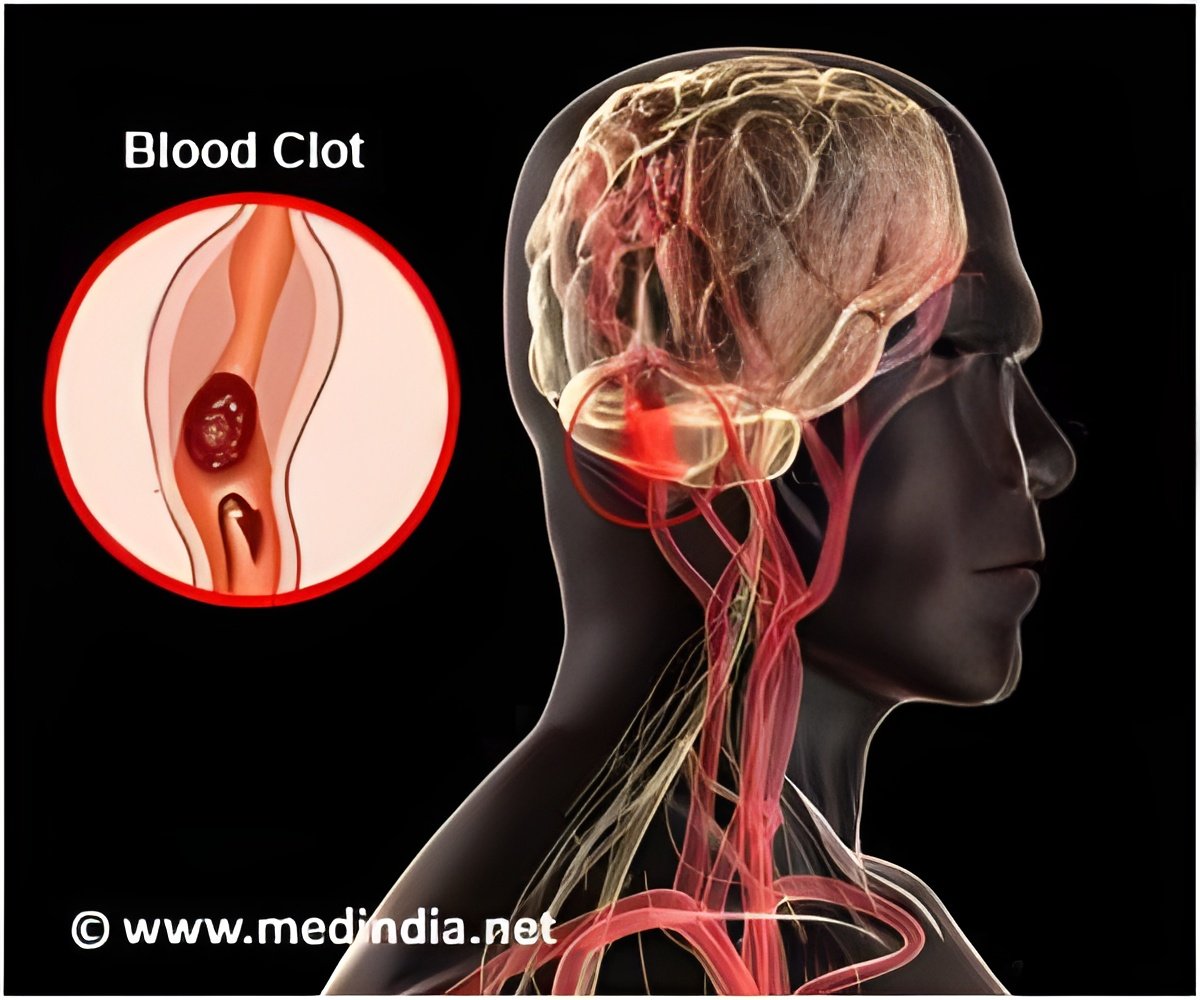
The researchers also conducted an analysis of independent predictors of stroke risk. Multiple regression analysis showed for the first time that each of the following factors independently reduced stroke risk: reperfusion therapy with percutaneous coronary intervention (PCI), blood clot dissolving therapy (fibrinolysis), thrombocyte aggregation inhibitors (aspirin and P2Y12-inhibitors) and statins. Dr Ulvenstam said: "The finding that PCI actually reduces stroke risk is somewhat surprising, being an invasive procedure. It has traditionally been associated with an increased stroke risk. We speculate that early reperfusion of the myocardium reduces infarction size and thereby leads to a reduced burden of atrial fibrillation and heart failure and in turn, reduced stroke risk."
Advertisement
Source-Eurekalert