Researchers identified activated T cells with anti-leukemic activity, advancing T cell therapies for leukemia.
‘Decoding #Leukemia Success: New research reveals distinct cellular patterns in patients who respond to donor #lymphocyte infusion therapy. #cancer #bloodcancer’





For patients with AML, a stem cell transplant holds the potential for a cure. The goal of the transplant is to replace the patient’s hematopoietic stem cells – cells that rejuvenate supplies of blood and immune cells – with donor stem cells that are not cancerous. In addition, the donor cells also include active immune cells that can attack leukemia cells that remain in the patient after the transplant. This phenomenon is called the graft versus leukemia effect. However, approximately one in three patients with AML relapse after allogenic stem cell transplant. DLI is a follow-on treatment that can help stave off or treat relapse. It involves an infusion of white blood cells, called lymphocytes, from the donor of the stem cell transplant into the patient.
What is Donor Lymphocyte Infusion
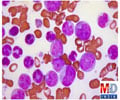
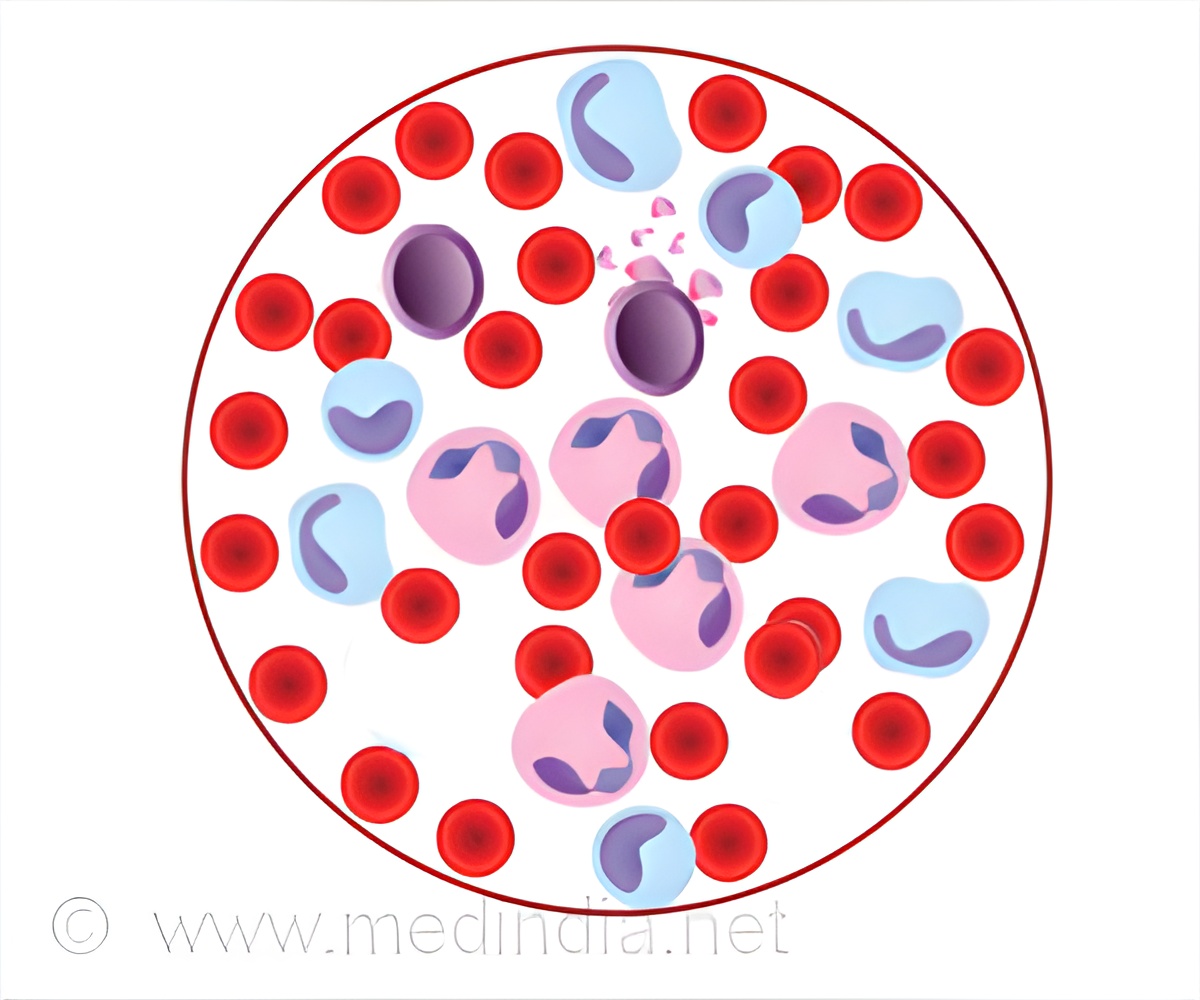
DLI is successful in only about 15-20% of patients with AML. Further, exactly how the cells in the DLI product help move leukemia into remission are not known, making it difficult for investigators to improve the treatment.Maurer and principal investigator Catherine Wu, MD, chief of Dana-Farber’s Division of Stem Cell Transplantation and Cellular Therapies, wanted to learn more about what factors contribute to the success of DLI. To do this, they examined cells from the bone marrow of 25 patients with relapsed leukemia who had been treated with stem cell transplant and DLI. The sample included patients who responded to DLI and patients who did not.
They employed single cell sequencing techniques to deeply profile multitudes of cells from each patient. This enabled the team to learn not only the range of cell types in the bone marrow, but also how those cells were interacting and driving immune responses in the patient.
Advertisement
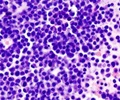
The team also identified a single immune cell type that appears to mediate the graft versus leukemia effect in patients that respond to DLI. The cell type, CD8+ cytotoxic T lymphocytes that express a transcription factor called ZNF683/Hobit at high levels, appear to coordinate with other immune cells to expand and attack leukemia cells. In patients who did not respond, these T cells had lower levels of expression of ZNF683/Hobit and higher levels of markers that inhibit their activity.
Advertisement
“The goal of our research is to identify the ways in which some patients respond, in the hopes that uncovering these mechanisms can help us create improved therapies that are more effective for a greater number of patients,” says Maurer.
Source-Eurekalert