Investigators at the Stanford University School of Medicine have developed a novel protocol that allows kidney-transplant recipients to jettison their indispensable
In all 12 cases, recipients were supplied with immunologically matched donor kidneys from close relatives. But the trial, which has been actively enrolling new patients, is now expanding to include imperfectly matched donor-recipient pairs as well.
"Transplant recipients can ordinarily expect to be on a regimen of two or three immune-system-suppressing drugs for the rest of their lives," said immunologist Samuel Strober, MD, who is a professor of medicine and the new protocol's inventor.
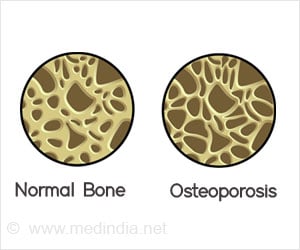
"While they help ward off rejection of the new organ by the patient's own immune system, these drugs carry their own risk of side effects, such as high blood pressure, diabetes and cancer," Strober said. The drugs themselves are somewhat toxic to the kidneys, although that is far outweighed by their value in preventing immune rejection.
Moreover, immune-suppressing drugs don't always work. In those cases, the patient experiences a gradual deterioration of the donated organ until it eventually fails, necessitating another transplant operation or a lifetime on dialysis.
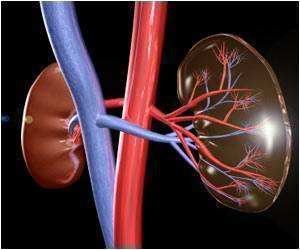
The new technique differs from the standard kidney-transplant procedure mainly by combining carefully targeted irradiation of a patient's lymph nodes, spleen and thymus — thus temporarily weakening their own immune systems — with the administration of stem cells drawn from the kidney donor's blood. These new donor cells eventually differentiate to join the components of a recipient immune system that is now much more "friendly" to the new organ than is observed in classical transplantation experience.
Advertisement
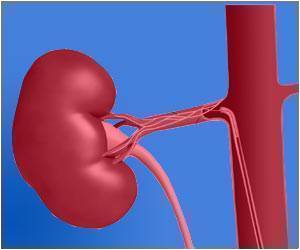
More than 400,000 people in the United States are on dialysis (mechanical filtration of the blood) for kidney failure. Dialysis, while life-extending, is far from a perfect solution. Patients must spend several hours immobilized in special centers three times a week for the rest of their lives or, less commonly, receive more frequent dialysis in home rigs. Moreover, life expectancy for patients on dialysis is significantly lower than for those who successfully receive new kidneys. Dialysis is also expensive, costing close to $70,000 per patient per year.
Advertisement
Left to itself, the patient's immune system would relentlessly attack a new organ unless it came from an identical twin. To stave off this attack, all transplant recipients are routinely placed on a regimen of immune-suppressing drugs. But in addition to their potential side effects, these drugs all too often fail to prevent organ rejection, which can be precipitous or gradual.
"Failure of a transplanted kidney is an expensive event," with an approximately $80,000 price tag to the health-care system during the year when the failure occurs, said Scandling.
The new protocol carries a total expense estimated to range from $20,000 and $40,000, so it has the potential to pay for itself within a few years. And it requires no additional hospital time.
Under the protocol, the kidney recipient receives radiation treatment and injections of antibodies while still in the hospital a few days after surgery, and additional radiation doses over the next several days on an outpatient basis. About 10 days after surgery, the recipient gets an injection of cells taken from the organ donor. All patients initially are put on two of the same immune-suppressing drugs (plus antivirals and antibiotics) that transplantation patients would normally get.
After a month, one of the drugs is withdrawn; thereafter, the Stanford team, led by Strober, continually monitors numerous parameters including the mixing of donor and recipient immune cells. If that mixing seems in balance six months after surgery, the recipient's second immunosuppressant-drug dose is discontinued. If the mixing hasn't been achieved, the patient remains on the drugs until it is.
At first the scientists thought the careful balancing act between the recipient's and donor's immune systems might need to remain intact permanently. But it now looks as though a gradual shift back toward predominance by the recipient's immune system, observed in a number of cases, doesn't cause organ rejection.
Recipients and donors in this trial are what immunologists call "a perfect match." They share identical versions of all six so-called HLA antigens, surface markers on every cell in a person's body. This lowers the risk that a patient's immune system will attack the transplanted organ. The trial — which has been funded by the National Institutes of Health — is now expanding to allow participation of recipient-donor pairs with as few as three matching HLA antigens. The study of perfectly matched pairs is continuing with philanthropic support from the Stanford Institute for Immunity, Transplantation and Infection. During the past year, four more perfectly matched patients received transplants, and three already stopped immune-suppressive drugs.
Source-Eurekalert