Countless Americans suffer from wounds that don't heal. Though majority are usually diabetes related, new research has recognized another likely underlying cause, ‘autoimmune diseases’.
So Shanmugam and her colleagues conducted a chart review of people who sought care at a high-volume wound clinic at Georgetown University Hospital to determine the prevalence of autoimmune diseases. The study included patients with open wounds — usually leg ulcers who were treated during a three-month period in 2009. Of the 340 patients, 49 percent had diabetes, which she says is a typical rate.
"But what was surprising is that 23 percent had underlying autoimmune diseases, and the connection between these relatively rare disorders and wounds that don't heal is under-recognized," she says.
Of the 78 patients in the cohort who had autoimmune disease, most had rheumatoid arthritis, lupus or livedoid vasculopathy, a type of vascular disease.
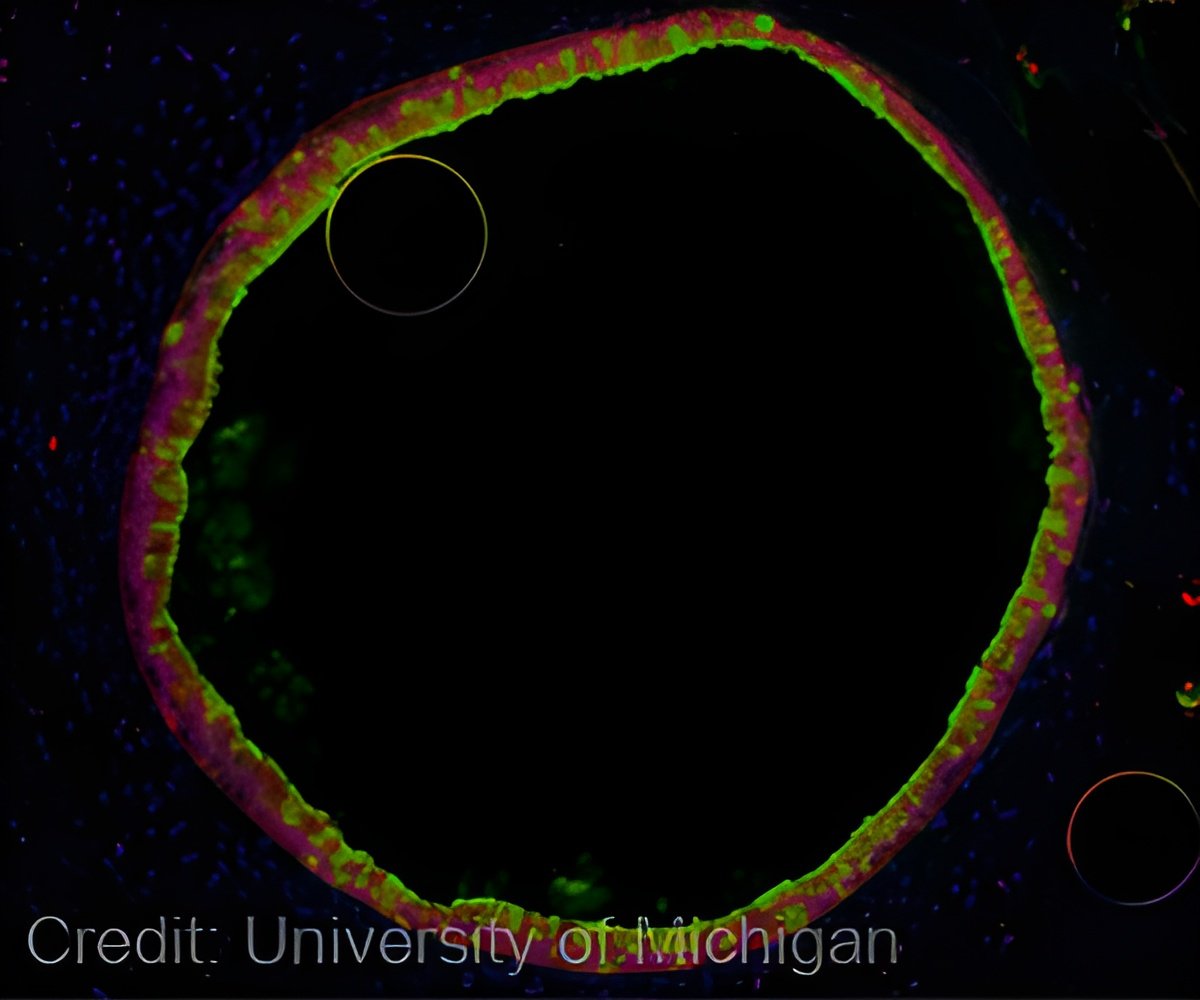
Shanmugam says her findings also show that autoimmune disease-associated wounds were significantly larger at the patient's first visit. These non-healing wounds can be "incredibly emotionally draining and financially costly," Shanmugam says, because they require doctor visits over many months as well as an ever-present risk of serious infections. Sometimes, infections can lead to surgery and the amputation of limbs. More often, they require skin grafts or use of skin substitutes, which may still not solve the problem.
In fact, Shanmugam's study found that skin grafts were more likely to fail in patients with autoimmune disease-associated wounds.
Advertisement
Source-Eurekalert