Researchers have shed more light on the formation of cutaneous lesions of meningococcal sepsis due to the adhesion of Neisseria meningitidis to human microvessels in a humanized mouse model.
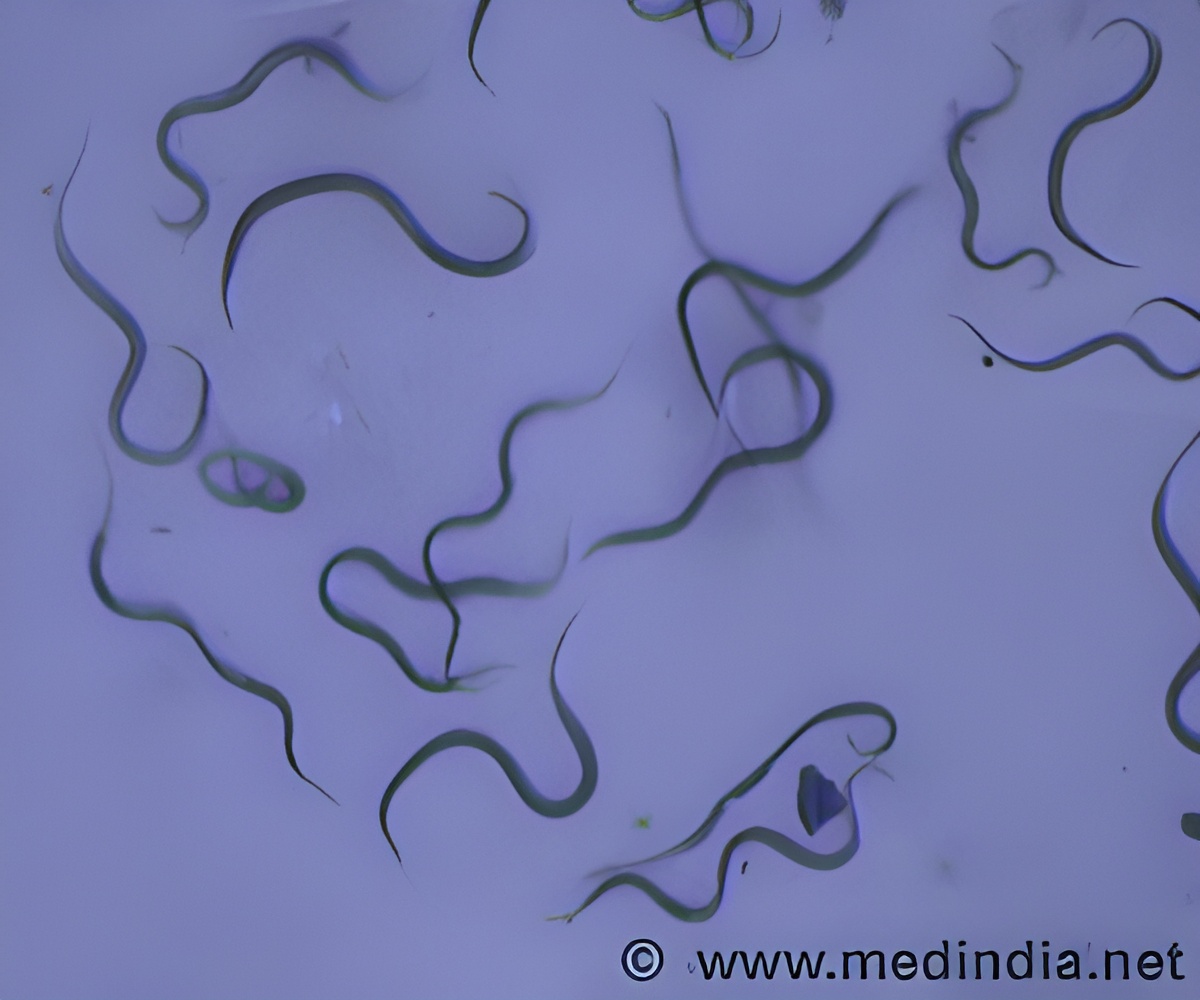
In this research, investigators utilized a humanized mouse model, where human skin, containing an abundance of human microvessels, was grafted onto immunocompromised mice. Grafted mice thus had a hybrid vasculature, part mouse, and part human. In this context, N. meningitidis associated exclusively, and in significant numbers, with the human vessels. Once associated with the human vessels the bacteria rapidly led to an endothelial inflammatory response with expression of the human pro-inflammatory cytokines IL-6 and IL-8 and the infiltration of inflammatory cells. Vascular events such as clotting, thrombosis, congestion and vascular leak were all observed in the infected human vessels, mimicking the clinical pathology. The combination of these factors led to the development of a purpuric rash in 30% of the infections. The association of the bacteria with the human vessels was shown to be dependent on the adhesive properties of the bacterial Type IV pili, filamentous structures found at the surface of many pathogenic bacteria. Importantly, bacterial mutants deficient for these adhesive structures do not lead to any distinctive pathology despite normal numbers of circulating bacteria.
This work thus leads to a change in the paradigm in our understanding of the disease mechanism, with local adhesion events now considered central to the disease process. Because it recapitulates key features of human infection, the described experimental model opens new avenues of research to further understand the mechanisms of disease and to design new prevention and treatment strategies.
Source-Eurekalert












