Increased levels of calcitriol in prostate tissue observed through elevated oral doses of plain vitamin D.
"This study shows calcitriol makes the foot come off the gas pedal of cancer growth. We are not able to prove that the speed of the car has slowed down, but it certainly is a good sign," said Vieth. "We expect that this early-phase clinical trial will open the door for more detailed clinical research into the usefulness of vitamin D in the treatment or prevention of prostate cancer."
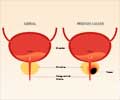
Vieth and colleagues previously reported that in men who were being monitored regularly for prostate cancer, higher vitamin D levels slowed the rate of rise in prostate-specific antigen levels. They randomly assigned 66 men scheduled for radical prostatectomy to daily vitamin D in doses of 400, 10,000 or 40,000 IU for three to eight weeks before surgery.
Researchers found that calcitriol levels in the prostate increased progressively with each daily dose of vitamin D, with 40,000 IU showing the highest levels. These higher levels of calcitriol corresponded with lower prostate levels of Ki67, a protein that indicates prostate cancer cell growth, as well as higher levels of specific growth-inhibitory microRNAs.
Vieth stressed that he and his colleagues do not advocate vitamin D supplementation in doses higher than 4,000 IU daily. Patients were assigned to the 40,000 IU daily dose because of the short presurgical time frame available for study, not as a regular regimen.
"Plain vitamin D provides the raw material to permit the body to take care of its own needs," he said. "We showed here that plain vitamin D allows the prostate to regulate its own level of calcitriol, and at the doses we used, for the time frame we used, it has been safe with the hoped-for desirable outcomes."
Advertisement
This research was funded by the Canadian Cancer Society and was a collaboration between investigators at University Health Network, Sunnybrook Hospital and Mount Sinai Hospital, all in Toronto, and at the University of Chicago.
Advertisement
Founded in 1907, the American Association for Cancer Research (AACR) is the world''s first and largest professional organization dedicated to advancing cancer research and its mission to prevent and cure cancer. AACR''s membership includes 34,000 laboratory, translational and clinical researchers; population scientists; other health care professionals; and cancer advocates residing in more than 90 countries. The AACR marshals the full spectrum of expertise of the cancer community to accelerate progress in the prevention, biology, diagnosis and treatment of cancer by annually convening more than 20 conferences and educational workshops, the largest of which is the AACR Annual Meeting with more than 18,000 attendees. In addition, the AACR publishes seven peer-reviewed scientific journals and a magazine for cancer survivors, patients and their caregivers. The AACR funds meritorious research directly as well as in cooperation with numerous cancer organizations. As the Scientific Partner of Stand Up To Cancer, the AACR provides expert peer review, grants administration and scientific oversight of individual and team science grants in cancer research that have the potential for patient benefit. The AACR actively communicates with legislators and policy makers about the value of cancer research and related biomedical science in saving lives from cancer.
Title: Double-blind randomized clinical trial of vitamin D3 showing effects on tissue calcitriol levels, gene expression and proliferation immunohistochemistry in prostate cancer.
Author Block: Dennis Wagner1, Larisa Nonn2, Angeline Antonio2, Avani Vaishnav2, Laurence Klotz3, Neil Fleshner4, Antonio Finelli4, Dominique Trudel4, Theodorus Van der Kwast4, Reinhold Vieth1. 1University of Toronto/Mount Sinai Hospital, Toronto, Ontario, Canada; 2University of Illinois at Chicago, Chicago, IL; 3Sunnybrook Health Sciences Centre, Toronto, Ontario, Canada; 4University Health Network, Toronto, Ontario, Canada.
Background: Preclinical data suggest that vitamin D plays a favourable role in prostate cancer prevention and prognosis, but its putative anticancer effects have not been validated in clinical prostate tissue samples. Here, we report the results from a randomized clinical trial (RCT).
Objectives: We conducted an RCT to determine whether simple cholecalciferol (vitamin D3) consumed orally elicits effects on prostate cancer pathology in prostate tissue obtained at surgery.
Methods: Prostate cancer patients (n=66) with Gleason scores 6 or 7 and scheduled for radical prostatectomy were randomized to daily vitamin D doses of 400, 10,000, or 40,000 IU for 3-8 wk before surgery.
Results: Laser-capture microdissected paraffin-embedded prostate tissue showed differential expression, between benign and cancerous regions, for the cancer-related mRNAs and miRNAs, as well as for the Ki-67 proliferation marker (p0.07 among groups). The group consuming 40,000 IU/d vitamin D exhibited the highest levels of both calcitriol and its precursor as measured in frozen prostate tissue and in serum (p<0.02 each). Prostate tissue calcitriol correlated strongly with the expression of androgen receptor mRNA (r = -0.58, p=0.001), NKX3.1 mRNA (r = -0.39, p=0.02), miR-100 (r = 0.44, p=0.01), miR-125b (r = 0.37, p=0.03), Let-7a (r = 0.47, p=0.03), miR-141 (r = 0.51, p=0.002), miR-106b (r = 0.45, p=0.01), and miR-331-3p (r = 0.47, p=0.005). Automated digital analysis of immunohistochemically stained prostate cancer regions showed that prostate tissue calcitriol related negatively with Ki67 intensity (r = -0.38, p =0.02) and percent of nuclei stained strongly positive (3+) for Ki67 (r = -0.41, p=0.008). A threshold effect was evident such that patients at the highest quartile of prostate tissue calcitriol (≥ 37 pmol/kg) had significantly lower AR mRNA (p<0.001), NKX3.1 mRNA (p=0.01), and Ki67 measures (p<0.05), as well as higher levels of the correlated miRNAs (p<0.05), compared to those with lower levels.
Conclusions: We provide level-1 clinical evidence that higher oral vitamin D doses produce higher levels of calcitriol within prostate tissue, and that higher prostate calcitriol relates to lower androgen receptor mRNA, higher miRNA signalling, and diminished expression of the proliferation marker Ki67 in prostate cancer. These RCT results justify a need to explore strategies that may maximize calcitriol within prostate for cancer chemoprevention.
Source-Newswise


![Prostate Specific Antigen [PSA] & Prostate Cancer Diagnosis Prostate Specific Antigen [PSA] & Prostate Cancer Diagnosis](https://images.medindia.net/patientinfo/120_100/prostate-specific-antigen.jpg)