Investigators develop advanced technology that can measure white blood cell activation and function, providing significantly more prognostic information about patients with sepsis.
‘Accurate diagnostic test for identifying the immune system's activity would enable clinicians to change their immune modulating therapies to maximize benefit and minimize risk for patients.’
Read More..




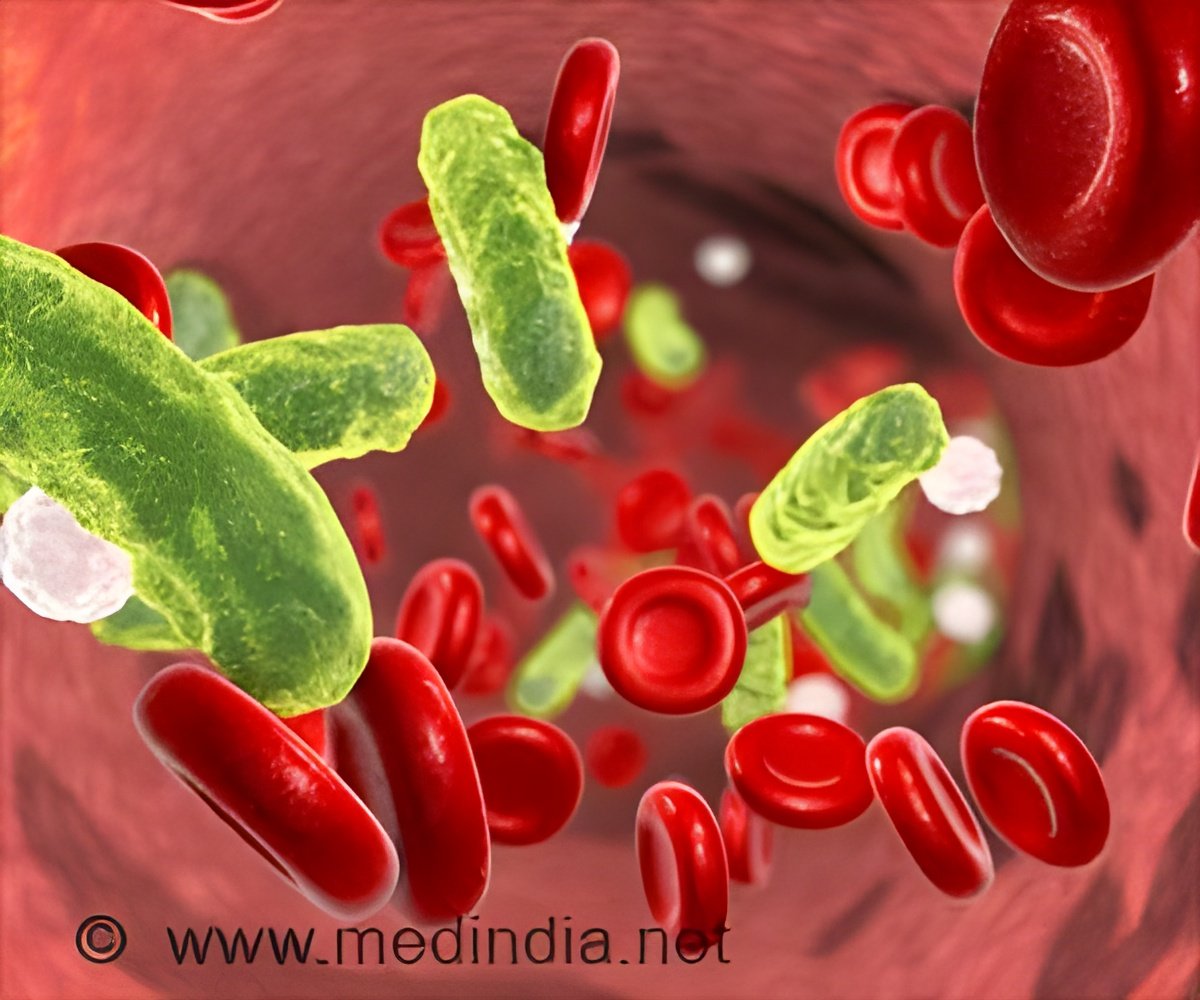
Most of the time, physicians can control the infection itself. What ultimately leads to multi-organ system injury and fatality is the patient's immune system's over-exuberant response. Current testing and bedside diagnostics do not provide clinicians with precise and timely information needed to rapidly change their therapeutic approach. Read More..
"Our idea was to develop a point-of-care diagnostic test that, instead of focusing on the white blood cell count, would inform us about white blood cell activation state and function," said corresponding author Bruce Levy, MD, chief of the Division of Pulmonary and Critical Care Medicine at the Brigham.
"It's been exciting for us, as translational scientists, to work on a solution with outstanding bioengineer colleagues. Together, we're able to address a truly important clinical problem."
The team's technological advancements are two-fold. The new approach uses microfluidics -- tiny channels that aligns cells by their size, allowing investigators to sort out larger white blood cells from smaller red blood cells and other elements of the blood.
This requires only microliter quantities of blood instead of milliliters -- in other words, drops of blood instead of vials of it. This sample sparing approach, in turn, could reduce the risk of iatrogenic anemia among patients.
Advertisement
The team assessed samples from 18 hospitalized patients and 10 healthy subjects, looking at the collected samples over the course of seven days. Both the activation state and function of white blood cells were significantly more predictive of the patient's clinical course than were white blood cell counts.
Advertisement
A more precise diagnostic test for the immune system's activity would enable clinicians to adjust their immune modulating therapies to maximize benefit and minimize risk for individual patients.
"We're excited to take the next steps forward," said co-first author Bakr Jundi, MD, MMSc, a researcher in the Levy lab. "As physicians try to understand how sepsis affects patients and how we can better monitor patients, we hope this technology will help to address some of the main issues clinicians face."
Source-Eurekalert