While CD4+ T cells are crucial in the immune response to pulmonary infections, an excess of these cells can lead to lung damage.

T cell-specific P2RX7 favors lung parenchymal CD4+ T cell accumulation in response to severe lung infections
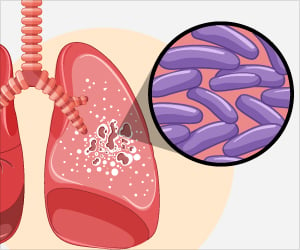
Go to source) The study described in the article involved infecting mice with hypervirulent tuberculosis and influenza. This finding opens up perspectives for therapeutic interventions aimed at combating diseases that attack the lungs, while not affecting the ability of the adaptive immune system to fight off infection. Even relatively small numbers of CD4+ T cells in the lungs proved sufficient to afford protection against tuberculosis, for example.
‘Achieving an "optimal quantity" of CD4+ T cells in the lungs was essential for curing tuberculosis and influenza. #lungdisease #lunginfection #tuberculosis’





The researchers found that amounts of these cells in lung tissue are mediated by a specific receptor called P2RX7, a protein primarily expressed in immune cells and capable of detecting the presence of extracellular adenosine triphosphate (ATP). The main functions of ATP relate to energy production for cells, but in response to stress or tissue damage it may be released into the external medium, acting as a danger signal for defense cells and potentially leading to an exacerbated response.
P2RX7 Activation Spurs CD4+ T Cell Accumulation Intensifying Lung Disease Severity
In such cases, P2RX7 induces an excessive buildup of CD4+ T cells and boosts expression of the chemokine receptor CXCR3 (chemokines are proteins that direct the migration of white blood cells to infected or damaged tissue). According to the article, the excessive buildup of CD4+ T cells in the mice’s lungs induced by activation of P2RX7 correlated with an increase in the severity of the disease and a reduced survival rate.“ATP in the extracellular medium is recognized by the immune system as a sign of damage because it should be inside the cell rather than outside. Previous research showed how important it is to the development of severe forms of tuberculosis, but the mechanisms weren’t understood. In particular, we didn’t know which type of cell expressed it most.
This was what we set out to investigate. We also wanted to find a way to improve the response of these T cells. What we didn’t expect was that removing the receptor to block recognition of ATP would lead to an improvement and not a deterioration,” Igor Santiago-Carvalho, first author of the article, told Agência FAPESP. He has a PhD in immunology and is a researcher at the University of São Paulo’s Biomedical Sciences Institute (ICB-USP) in Brazil.
Santiago-Carvalho’s work was supervised by Maria Regina D’Império Lima, first author of the article and a professor at ICB-USP. She has been researching cellular immunology for 20 years, mainly in malaria, Chagas disease and tuberculosis.
“The more we know about the factors that determine whether the immune response is deficient, optimal or excessive, the better we’ll be able to manipulate it with drugs and treatments to control and even cure the disease,” Lima said.
Advertisement
“We were particularly concerned with ATP, and we found that the inflammatory response is intense and harmful when an excessive amount of T cells enter the tissue as they detect ATP. In some cases, it results in pulmonary fibrosis. Intervening in this signaling pathway could be an effective way to reduce the damage done by an excessive immune response to infection.”
Advertisement
- A deep learning algorithm to predict risk of pancreatic cancer from disease trajectories - (https://linkinghub.elsevier.com/retrieve/pii/S2211124723014602)