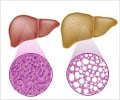
A mechanism by which the good bacteria that reside in our gastrointestinal tract can help protect us from inflammation, and how their disruption (dysbiosis) can increase the susceptibility of the liver to more harmful forms of disease identified.

‘Inflammatory response in fatty liver disease is reduced by two tryptophan metabolites from gut bacteria.’





"That's bad news for the liver," said Kyongbum Lee, Ph.D., professor of chemical and biological engineering at the School of Engineering at Tufts. "We demonstrated that two of these metabolites - I3A and TA - attenuate the effects of inflammation in several ways. Their depletion clears the way for disease to progress toward more serious stages."
Some of those effects of I3A and TA include reducing the level of inflammation-inducing molecules (known as cytokines) like tumor necrosis factor alpha, interleukin-1-beta, and monocyte chemoattractant protein. The latter acts as an attractant for macrophages, which in turn produce more cytokines. All of these inflammatory agents are triggered by high levels of free fatty acid accumulation in the serum and liver - the hallmark of NAFLD, and the consequence of an unhealthy high fat diet. Researchers also considered whether I3A and TA could be added back to the gut to help treat those with the more serious inflammatory stages of NAFLD. However, it was determined that high levels of TA are toxic. "Our focus now is on I3A, where we will be exploring whether I3A or other microbiota metabolites can change the course of disease," said Lee.
Source-Eurekalert