Mechanisms that prevent people from having an inflammatory response to harmless environmental exposures could also all allow cancer cells to spread to lungs.
‘Blocking the oxygen-sensing proteins of their T cells, could enhance T-cell responses against cancer and limit metastasis to the lung.’





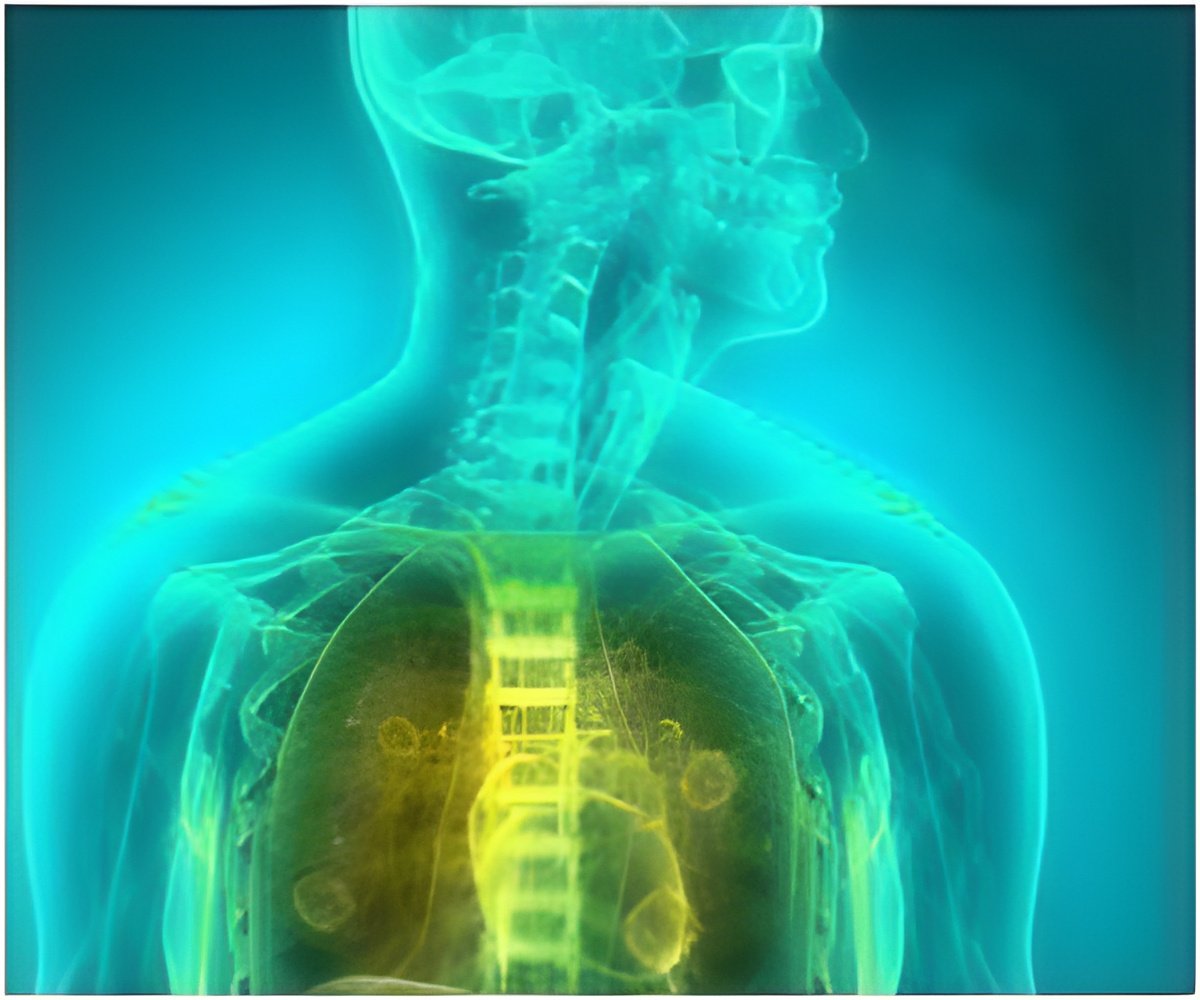
Cancer cells must break through normal immune defenses in order to spread to other parts of the body. Little is known, however, about the mechanisms that lead to cancer's spread to the lungs. Nearly 90% of cancer deaths occur when cancer spreads to a different part of the body -presenting a major obstacle to curative treatment. The lungs are a common site of metastasis for primary bladder, breast, colon, kidney, melanoma, ovary, pancreas, bone, rectal, stomach, thyroid, uterine and lung cancer.In this new study, researchers describe how oxygen functions as an immune system checkpoint to create an environment that enables cancer's spread to the lung more easily.
"Every time we take a breath, we bring things into our lungs that could produce a pretty dramatic and potentially harmful immune response - but the majority of the time they don't because in a normal, healthy state our immune systems are set up to accommodate for this," explains David Clever, PhD, first author of the manuscript and a current medical student at Ohio State. Clever completed this research under the mentorship of Nicholas Restifo, MD, of National Cancer Institute (NCI) during the doctoral portion of his Medical Scientist Training Program.
"The same 'normal' mechanisms put in place to suppress immune responses against harmless material taken into the body during the act of breathing can also suppress immune responses to the colonizing cancer cells that lead to metastatic tumors in the lungs. This creates an immunologically favorable niche - meaning the environment is prime for cancer cells to slip through the immune system's defenses, thrive and grow in the lungs."
Specifically, the team discovered that certain oxygen-sensing proteins (PHD cells) function to limit inflammation by T cells, a type of immune cell capable of killing cancer cells. In the highly oxygenated lung microenvironment the oxygen-sensing PHD proteins limit immune responses against cancer cells which opens the lung up as a fertile ground for metastasis.
Advertisement
These results contribute a new immunological basis for the predisposition of many cancers to metastasize to the lung that could help scientists develop new therapies to prevent the spread of cancer to the lungs.
Advertisement
Source-Medindia














