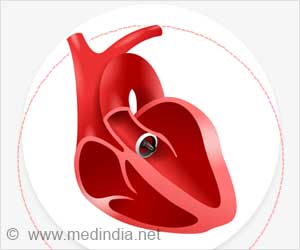
Researchers find procedure to be ‘risky and costly’ and call for better regulation and transparency on the use of such high-risk medical devices.

Since its introduction 10 years ago, around 40,000 procedures have been carried out worldwide.
TAVI is classed as a medical device. In Europe this means it needs only a simple quality certificate (CE mark) to gain access to the market, putting TAVI on the same footing as domestic appliances such as toasters. In contrast, the US Food and Drug Administration (FDA) demands trial evidence before it can license any innovative device. Thus TAVI was in use in Europe four years before the US.
However, guidance from the UK National Institute for Health and Clinical Excellence (NICE) says that the evidence for TAVI in patients who are suitable for conventional surgery is "inadequate."
The authors agree. After rigorous analysis of all the available data, combined with a study of real world TAVI practice in Europe, they conclude that "the arguments supporting the widespread use of TAVI do not stand up to scrutiny."
They also raise concerns about access to full trial data on TAVI and a lack of disclosure of financial interests among trial investigators.
Advertisement
They also call for a major improvement in transparency of information "to allow clinicians to practise evidence based medicine, patients to make informed decisions, and health technology assessment agencies to make the right judgements."
Advertisement