Researchers at the University of Pittsburgh Cancer Institute (UPCI) and the School of Medicine had identified the viral roots of a rare skin cancer

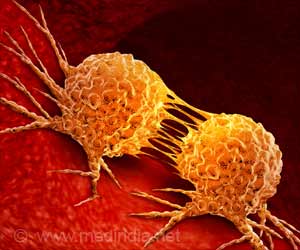
Merkel cell carcinoma (MCC), a skin cancer that is more common among seniors and those with weakened immune systems, could not be readily diagnosed at one time, and it still has a very poor prognosis, said Patrick S. Moore, M.D., M.P.H., and Yuan Chang, M.D., both of the Cancer Virology Program at UPCI and senior authors of a study that appears online today in Science Translational Medicine.
"This research effort shows the speed at which genomics can identify molecular causes for cancer and then point the way toward a rational and targeted treatment," Dr. Moore noted. "Since the inception of the 1971 U.S. National Cancer Act, researchers have strived to discover the underlying problems that trigger tumor development."
In 2008, the team first described the new Merkel cell polyomavirus (MCV) in Merkel cell carcinoma. Within a year, they showed it was responsible for tumor development in most cases of the disease. At least four out of five healthy adults world-wide are infected with MCV, which usually doesn't cause any symptoms.
"The virus remains in the skin cells, and in most cases, no damage is done," Dr. Chang said. "But when mutations occur to this virus, it can cause cancer. Most of the 1,500 new MCC cases per year in the U.S. are caused by MCV infection."
In quick succession, the team devised tests to identify virus-induced MCC, and began unraveling the biochemical pathways that encourage tumor formation. In their latest project, they "knocked out" a key viral protein called T antigen and found that MCV directly elevates a cellular protein called survivin.
Advertisement
A multicenter clinical trial of YM155, a still-experimental anti-cancer drug that is made by Deerfield, Ill.-based Astellas, is expected to begin in the next six months to determine its effectiveness in MCC patients. The trial will be led locally by Pitt School of Medicine assistant professor Hussein Tawbi, M.D., Ph.D., and professor John Kirkwood, M.D., who also is co-leader of the UPCI Melanoma Program, through the Eastern Cooperative Oncology Group, a multicenter cooperative group supported by the National Cancer Institute (NCI), part of the National Institutes of Health.
Advertisement
"Scientists can now quickly come up with answers to complex problems, like cancer, using human genetics," Dr. Moore noted. "In less than five years, we have gone from knowing very little about MCC to knowing its exact cause and are devising new, precisely targeted and less-toxic therapies."
Dr. Moore also is a Distinguished Professor and American Cancer Society Professor, Department of Microbiology and Molecular Genetics. Dr. Chang also is a Distinguished Professor and American Cancer Society Professor, Department of Pathology. Last week, they were elected to membership in the prestigious National Academy of Sciences. Prior to their work on MCV, the Chang and Moore lab team discovered another virus, a new human herpesvirus, in 1994 that causes Kaposi's sarcoma, the most common cancer among AIDS patients.
Source-Eurekalert