Cancer chemotherapy is not effective in treating cancer efficiently due to its non-specificity and inability to target the cancer cells alone.
Cancer chemotherapy is not effective in treating cancer efficiently due to its non-specificity and inability to target the cancer cells alone. Due to this non-specificity there is increased development of drug resistance shown by these cancer cells.
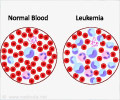
Normal cells and cancer cells depend on blood supply for sustenance and oxygen. Cutting off blood supply could be one way to kill the cancer cells. This is however fraught with problems as cancer cells have a propensity to create new blood vessels. Anti-angiogenesis drug prevents formation of development of new blood vessels. This process of cutting off blood supply is called anti-angiogenesis.Combining the two methods — chemotherapy and anti-angiogenesis — can be another way to kill cancer cells. This has it own limitations though — drugs that cut off blood supply not only deprive cancer cells of oxygen but also chemotherapy drugs that can kill the cancer cells.
`Nanocells' (of 200 nanometres in size) in a balloon within a balloon design — to deliver chemotherapy agents and drugs for destroying the blood supply to the cancer cells. The outer balloon has the anti-angiogenesis agent and the inner balloon has chemotherapy drugs.
"We tried the other combination but it will not work out," Dr. Sasisekharan explained. "First you need a vascular shut down (blood supply cut off) and then release the chemotherapy drug.”This will not only increase the therapeutic index but also decrease the toxicity. And this will happen only if the outer balloon is filled with an anti-angiogenesis drug."
The ability of the `nanocells' to wreak complete destruction of cancerous cells is aided by the cancerous cells themselves. "Tumour vessels suck things into their environment and the nanocells get trapped in the tumour bed due to their large size," he elucidated. The size of the nanocell plays a crucial role. While the 200 nanometre size of the nanocell prevents it from coming out of the blood vessel into organs, at the site of tumour it is a different story.
"Here the blood vessels are leaky and have pores as large as 400-600 nanometres," he noted. "So the nanocells can pass through the vessels into the tumour where they are retained." In other words Dr. Sasisekharan and his team used the difference in pathology of blood vessels in the tumour and the normal organs to selectively deliver the drugs.
Advertisement
"It may not be optimal to release the anti-angiogenesis and chemotherapy drugs simultaneously as the chemotherapeutic drugs may leak out before the blood vessels inside the tumour are cut," he elucidated.
Advertisement
The team had worked on animal models to treat melanoma and Lewis lung cancer. "There is no universal chemotherapeutic agent — they are dependent on the cancer," he observed. "We need to find the right combination of drugs that will work for a given tumour." Eighty per cent of mice treated with nanocells survived beyond 65 days compared with 30 days in the case of mice treated with the best current therapy. "The 65-day period wasn't a benchmark," he noted. "When we started this study, we did not expect the animals to survive this long."