Biofilms have been linked to 80% of infections, forming on living tissues or or dwelling in medical devices.
‘Biofilm-based infections are resistant to antibiotics, which makes it difficult to treat and it causes chronic inflammation, impaired wound healing.
’





"Chronic biofilm-based infections are often extremely resistant to antibiotics and many other conventional antimicrobial agents, and have a high capacity to evade the body's immune system," said Boyer. "Our study points to a pathway for the non-toxic dispersal of biofilms in infected tissue, while also greatly improving the effect of antibiotic therapies." Biofilms have been linked to 80% of infections, forming on living tissues (eg. respiratory, gastrointestinal and urinary tracts, oral cavities, eyes, ears, wounds, heart and cervix) or dwelling in medical devices (eg. dialysis catheters, prosthetic implants and contact lenses).
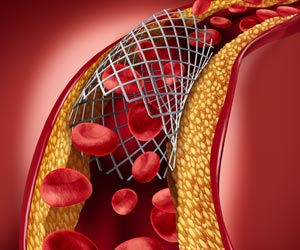
The formation of biofilms is a growing and costly problem in hospitals, creating infections that are more difficult to treat -- leading to chronic inflammation, impaired wound healing, rapidly acquired antibiotic resistance and the spread of infectious embolisms in the bloodstream.
They also cause fouling and corrosion of wet surfaces, and the clogging of filtration membranes in sensitive equipment -- even posing a threat to public health by acting as reservoirs of pathogens in distribution systems for drinking water.
In general, bacteria have two life forms during growth and proliferation: planktonic, where bacteria exist as single, independent cells; or aggregated together in colonies as biofilms, where bacteria grow in a slime-like polymer matrix that protects them from the environment around them.
Advertisement
Although biofilms were first recognised in the 17th century, their importance was not realised until the 1990s, when it became clear that microbes exist in nature more often in colonies made up of lots of different microorganisms that adhere to surfaces through slime excreted by their inhabitants. Thus began a global race to understand biofilms, at a time when it was also realised they were responsible for the majority of chronic infections.
Advertisement
When biofilms want to colonise a new site, they disperse into individual cells, reducing the protective action of the biofilm. It is this process the UNSW team sought to trigger, making the bacteria again susceptible to antimicrobial agents.
The UNSW team found that by injecting iron oxide nanoparticles into the biofilms, and using an applied magnetic field to heat them -- which induces local hyperthermia through raising the temperature by 5°C or more - the biofilms were triggered into dispersing.
They achieved this using iron oxide nanoparticles coated with polymers that help stabilise and maintain the nanoparticles in a dispersed state, making them an ideal non-toxic tool for treating biofilm infections.
"The use of these polymer-coated iron oxide nanoparticles to disperse biofilms may have broad applications across a range of clinical and industrial settings," said Boyer, who in October was named Physical Scientist of the Year in Australia's Prime Minister's Prizes for Science.
"Once dispersed, the bacteria are easier to deal with - creating the potential to remove recalcitrant, antimicrobial-tolerant biofilm infections."
Source-Eurekalert