Researchers measured how often generally healthy Medicare enrolees died in the seven days after being discharged, by tracking over 16 million visits to EDs.

‘Patients discharged with a diagnosis of confusion, shortness of breath, or generalized weakness were more likely to die, while those with chest pain were at significantly lower risk.’





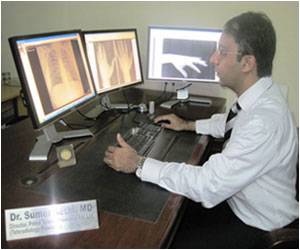
The findings are published in the February 1 edition of the British Medical Journal. "There's a lot of policy interest in reducing unnecessary admissions from the ED," said Ziad Obermeyer, MD, MPhil, a staff physician in the Department of Emergency Medicine at BWH. "We know that hospitals vary a lot in how often they admit patients to the hospital from the ED, but we don't know whether this matters for patient outcomes."
Researchers found that, each year, about 10,000 generally healthy patients die in the seven days after discharge from the ED. Heart disease and COPD were the most common causes of death, but narcotic overdose was also a leading cause, largely after visits for pain and injuries.
These early deaths were concentrated in hospitals that admitted few patients to the hospital from the ED, hospitals that are often viewed as models by policy makers because of their low costs. By contrast, deaths were far less frequent in large, university-affiliated EDs with higher admission rates and higher costs, even though the population served by these EDs was generally less healthy when they walked in the front door of the ED.
Patients discharged with a diagnosis of confusion, shortness of breath, or generalized weakness were more likely to die, while those with chest pain were at significantly lower risk. Researchers analyzed data from Medicare claims that covered ED visits from 2007-2012 to identify patients who died in the week after discharge. Patients with known serious illnesses or diagnoses of life threatening conditions in the ED and those over 90 years old, or receiving palliative care were excluded.
Advertisement
Source-Eurekalert