Bedaquiline, a new TB antibiotic, has proven effective against multidrug-resistant strains.

The findings of the study are published in the journal Nature Communications (1✔ ✔Trusted Source
Catalase activity deficiency sensitizes multidrug-resistant Mycobacterium tuberculosis to the ATP synthase inhibitor bedaquiline
Go to source).
“Understanding how a drug works could help us design new molecules that work better and prevent bacteria from becoming resistant,” said Jason Yang, assistant professor at the medical school and senior author of the study.
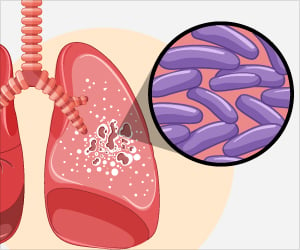
Tuberculosis still ranks among the world’s deadliest infectious diseases, killing more than 1.5 million people annually. Multidrug-resistant TB, defined as disease that is resistant to at least two first-line drugs, poses a rising threat to global TB control efforts.
‘Did You Know?
Tuberculosis remains one of the world’s leading infectious killers, claiming over 1.5 million lives each year. #TB #Tuberculosis #medindia’





Tuberculosis remains one of the world’s leading infectious killers, claiming over 1.5 million lives each year. #TB #Tuberculosis #medindia’
Advertisement
Bedaquiline: A New Weapon Against Drug-Resistant TB
Approved in 2012 by the U.S. Food and Drug Administration (FDA), bedaquiline was the first new TB drug in more than 40 years. It works well against multidrug-resistant TB strains, but the mechanisms behind its effectiveness weren’t fully understood.The findings could help spur TB treatment and drug development. Understanding these vulnerabilities could inspire strategies for making bedaquiline more effective, potentially allowing for lower doses or shorter treatment times. It also could also guide the development of new drugs or drug combinations.
“We can prevent resistance by developing other drugs that make bedaquiline work better,” Yang said. For example, combining bedaquiline with another antibiotic called isoniazid appeared to prevent the development of resistance to either drug, he said.
Advertisement
Lung Health at Risk: The Silent Spread of Tuberculosis
While TB is primarily a problem in developing countries, it remains a concern globally. Outbreaks still occur in the United States, though. There were, for example, about 500 cases in New York City last year.“TB itself is a ridiculously important problem right now, and so is antibiotic resistance," Yang said. “There was just a new report in the Lancet projecting if antibiotic resistance becomes worse, then we can't treat infections, and if we can't treat infections, much of modern medicine dies. You couldn’t even do surgery because surgical infections would kill patients (2✔ ✔Trusted Source
Global burden of bacterial antimicrobial resistance 1990 - 2021: a systematic analysis with forecasts to 2050
Go to source).”
Mycobacterium Tuberculosis: The TB Culprit
Researchers in the study, published in Nature Communications, examined both clinical isolates and laboratory strains of Mycobacterium tuberculosis, the bacteria that causes TB. The researchers used a systems biology approach, combining genetic studies, RNA sequencing and metabolic modeling.How Do katG Mutations Impact TB Drug Resistance and Susceptibility?
They found that deficiencies in an enzyme called catalase-peroxidase, encoded by a gene called katG, make drug-resistant TB more susceptible to bedaquiline. Mutations in katG are the most common cause of resistance to isoniazid, a first-line TB drug.This catalase deficiency leads to several changes that make the bacteria more vulnerable to the newer drug. It increases the accumulation of reactive oxygen species and susceptibility to DNA damage while changing transcriptional programs that regulate the bacteria's biology and repressing several biosynthetic pathways.
“We discovered some previously unreported mechanisms,” Yang said. “We show that these are the different kinds of vulnerabilities in TB biology or TB physiology that occur specifically in drug-resistant TB.”
The research also highlights potential avenues for repurposing existing drugs. Researchers found that trimethoprim and sulfamethoxazole, antibiotics used to treat other diseases, were also effective against drug-resistant TB strains with catalase deficiency.
The new paper was one of a related pair that appeared in Nature Communications from the same team. The second paper used whole genome CRISPRi screening to identify druggable vulnerabilities in a treatment-resistant strain of the disease (3✔ ✔Trusted Source
Whole genome CRISPRi screening identifies druggable vulnerabilities in an isoniazid resistant strain of Mycobacterium tuberculosis
Go to source).
Looking ahead, Yang and his colleagues are pursuing several lines of research building on these findings.
“We're developing machine-learning tools to understand other changes that are occurring in TB biology or TB physiology caused by other kinds of drug resistance,” Yang said. “We're extending those machine-learning models to see if we can extrapolate the findings from a laboratory setting directly into patients and clinical strains.”
This could potentially lead to personalized medicine approaches for TB, tailoring treatments based on the specific characteristics of the infecting strain.
The team is also developing synthetic biology tools to study how TB evolves drug resistance and how this process might be targeted to prevent resistance to bedaquiline and any new drugs that are developed.
References:
- Catalase activity deficiency sensitizes multidrug-resistant Mycobacterium tuberculosis to the ATP synthase inhibitor bedaquiline - (https://www.nature.com/articles/s41467-024-53933-8)
- Global burden of bacterial antimicrobial resistance 1990–2021: a systematic analysis with forecasts to 2050 - (https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(24)01867-1/fulltext)
- Whole genome CRISPRi screening identifies druggable vulnerabilities in an isoniazid resistant strain of Mycobacterium tuberculosis - (https://www.nature.com/articles/s41467-024-54072-w)
Source-Eurekalert