Researchers at the University of Maryland School of Medicine has identified a cell signaling pathway which plays a significant role in causing developmental defects of the fetal spinal cord and brain in babies of women with diabetes.

"Providing the best possible care for women before and during early pregnancy is a significant challenge because the first trimester is such a crucial time of development, and many women may not be aware that they are pregnant," says Dean E. Albert Reece, M.D., Ph.D., M.B.A., vice president for medical affairs at the University of Maryland and the John Z. and Akiko K. Bowers distinguished professor and dean of the School of Medicine. "Prenatal care is especially important for women who have diabetes because research has shown that even transient increases in blood glucose can lead to serious, and sometimes life-threatening, birth defects."
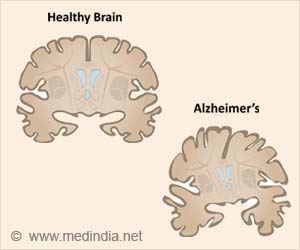
According to the U.S. Centers for Disease Control and Prevention, approximately 1 in 33 babies in the United States are born with a birth defect. Neural tube defects (NTDs), which occur when the fetal spinal column does not close completely in the first trimester, are among the most common type of birth defects and affect about 3,000 pregnancies each year. Women with diabetes prior to pregnancy are 3- to 10-times more likely to have a child with NTDs than women without disease. Folic acid (vitamin B; folate) has been shown to prevent NTDs in approximately 70 percent of pregnancies, but is not effective for everyone.
"Recent studies have reported that too much folic acid during pregnancy may increase risk of breast cancer in offspring later in life, so it has become increasingly important to find additional or adjunctive therapies to prevent NTDs," says Peixin Yang, PhD, associate professor in the Department of Obstetrics, Gynecology and Reproductive Sciences, who led the current study. "For women with diabetes, whose risk of having an infant with a birth defect is much higher than in the general population, having additional preventive methods could significantly improve a baby's development."
Previous work has revealed that a cell signaling pathway which leads to programmed cell death, known as apoptosis, greatly contributes to NTDs. High levels of maternal glucose in diabetic pregnancies lead to abnormal cell death during fetal development. Although much of this work has been conducted in animal models of diabetic pregnancy, and performed by research teams led by Dean Reece, the authors also confirmed that the same pathway is present in human fetal tissues with NTDs.
In the current study, investigators under the direction of Dr. Yang and Dean Reece at the University of Maryland School of Medicine, observed that high levels of glucose initiate the apoptotic pathway by activating a protein called apoptosis signal-regulating kinase 1 (ASK1). Once activated, ASK1 turns on a cell death pathway by activating other pro-cell death proteins. The team found that reducing ASK1 activity, either by deleting the Ask1 gene or by giving diabetic pregnant mice an ASK1 inhibitor, also reduced the incidence of NTDs.
Advertisement
One of the most promising results from this study is that the ASK1 inhibitor the team used is a small protein called thioredoxin which people naturally produce. Thioredoxin is thought to act as an antioxidant and has been used commercially as an anti-aging agent in some cosmetics.
Advertisement
"This work contributes greatly to our understanding of how high blood glucose causes birth defects and identifies specific targets that could be exploited to prevent diabetes-induced NTDs," says Dr. Reece. "The findings on thioredoxin's inhibitory effects also have implications for other diseases, such as cancer or kidney disease, which are caused or exacerbated by cell death."
Source-Eurekalert