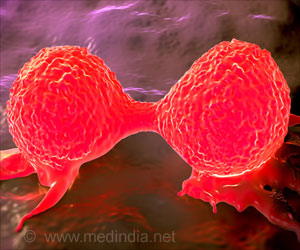
Research indicates that in their lifetime, women have more than a 12 percent risk of being diagnosed with breast cancer

Existing breast cancer treatments don't work for everyone, and alternative methods and delivery systems for breast cancer treatment are critical to saving and improving patient lives. New approaches to be presented at Era of Hope include research that explores using reconstituted "good" cholesterol as a drug delivery model as well as a study looking at a heat-activated drug delivery system using peptides to target tumors.
"The Department of Defense Breast Cancer Research Program is proud to support the investment into early and new science that can potentially improve and enhance the lives of breast cancer patients," said Captain Melissa Kaime, M.D., Director of the Congressionally Directed Medical Research Programs (CDMRP), under which the BCRP is managed. "The Era of Hope conference provides an opportunity for investigators to share the results of their research and collaborate about next steps, ultimately striving to make a significant impact in the lives of breast cancer patients."
Thermally Targeted Delivery of a c-Myc Inhibitory Peptide in Vivo Using Elastin-like Polypeptide
Principal Investigator: Gene Leflore Bidwell, III, PhD, University of Mississippi Medical Center
Surgery, along with chemotherapy and radiation are traditional treatment methods for breast cancer, but the harm to normal tissue, tumor metastasis and resistance to treatment can hinder a successful outcome. Thus, it is critical to identify alternative targeted approaches that reduce undesired side effects. Researchers at the University of Mississippi Medical Center developed a polypeptide (CPP-ELP-H1) that is responsive to heat and inhibits breast cancer cell growth by blocking the activity of c-Myc, an oncogenic protein.
The polypeptide is comprised of cell-penetrating peptide (CPP) and elastin-like peptide (ELP). When administered systemically, ELPs remain soluble and are cleared from circulation at normal body temperature. But at the tumor site, where mild heat is applied externally, ELP aggregates and accumulates. The CPP then facilitates entry into the tumor cells, where H1, an inhibitory peptide, blocks c-Myc activity.
Advertisement
"What's novel about our work is we're developing a carrier for peptide therapeutics," said Dr. Gene Leflore Bidwell of University of Mississippi Medical Center. "Peptides are easier to rationally design for a specific target than small molecules are. You can design peptides to modulate pathways of interest for certain types of breast cancer, but the problem with peptides is they need carriers to be made into good drugs. We generated a carrier to do that using thermal targeting, so the carrier we use specifically responds to heat."
Advertisement
Principal Investigators: Andras Lacko, PhD and Nirupama Sabnis, PhD, University of North Texas Health Science Center, Fort Worth
In the United States, six percent of women with breast cancer already have metastatic disease at the time of diagnosis.2 Despite improved response rates to currently available treatments, drug resistance continues to be an issue. A multi-site study was conducted to investigate a highly innovative approach for selectively targeting breast cancer by using biocompatible nanoparticles.
Researchers developed a novel drug delivery model utilizing synthetic and reconstituted high-density lipoprotein (rHDL) or good cholesterol nanoparticles that is uniquely effective in selectively encouraging cancer cells to accept therapeutic treatments. The anti-cancer agent used in the study was siRNA directed against the STAT-3 transcription factor and focal adhesion kinasse (FAK). 3 The drug carrying the nanoparticles was 20 times more efficient in suppressing the growth of breast cancer cells than the drug on its own, and in vivo studies in mice led to the suppression of the growth of human breast tumors by more than 70 percent. The system targets malignant cells and tumors via the scavenger receptor type B1 (SR=B1). The normal function of the SR-B1 receptor includes the extraction of cholesteryl esters from high density lipoproteins (HDL). This receptor has been shown to be markedly overexpressed in malignant cells and tissues, apparently because of their need for excess cholesterol due to their high proliferative rates. Researchers have found the SR-B1 receptor is also the major gateway for the entry of anti-cancer drugs into malignant cells. During the study, the accumulation of the siRNA (delivered via the rHDL nanoparticles) was undetectable in nearly all normal tissues, while it was substantial in tumor tissue, suggesting the selective drug delivery to tumors via rHDL is feasible.
"This novel drug delivery system has the potential to be compatible with most of the commonly used chemotherapy agents," said Dr. Andras Lacko of University of North Texas Health Science Center, Fort Worth. "This is a selectively targeted model, so cancer cells are reached, and normal cells are spared. We hope to contribute to what could bring patients a more effective therapy with reduced side effects."
Therapeutic Eradication of DCIS Progenitor Cells
Principal Investigator: Lance A. Liotta, MD, PhD, George Mason University
The true malignant nature of ductal carcinoma in situ (DCIS), breast cancer that begins inside the milk ducts 4, remains unclear, and therefore, it is often considered difficult to treat. A collaborative study led by Dr. Lance A. Liotta of George Mason University with Dr. Kirsten Edmiston of Inova Health System and Virginia Espina of George Mason University was conducted to answer the question: When does the propensity for breast cancer invasion first begin? Researchers also sought to investigate the potential of autophagy, a cell survival mechanism used by DCIS malignant progenitor cells growing within the breast duct, as a novel target for treating this type of disease.
In this study, an initial culture sample of fresh human DCIS lesions was shown to elicit cells with full malignant, or cancerous, properties in an animal model. Some of these cancerous properties include invasion, spheroid formation, and the ability to produce more tumors or tumorigenicity. Treatment with a lysosomotropic inhibitor of autophagy (chloroquine phosphate [CQ]) reversed all the invasive and tumorigenic properties, induced cell death and eliminated genetically abnormal cells from the organ culture.5 The mechanism of the suppression was the inhibition of autophagy. Findings indicate that the malignant cells are surviving within the breast duct by using autophagy to digest cell components in lysosomes and generate energy.6 Lysosomotropic inhibitors 7 work by modifying lysosomal function and reducing the cell survival mechanisms employed by malignant cells.
"Based on our findings, we are testing the safety and effectiveness of CQ in patients with DCIS," said Dr. Lance Liotta. "This trial will investigate the applicability of autophagy as a novel treatment target for DCIS, and if successful, could provide a neoadjuvant therapy option for this difficult to treat disease and a new approach to prevent breast cancer by killing preinvasive lesions."
Source-Eurekalert