A new study shows that magnetic resonance imaging (MRI) has been shown to reduce overdiagnosis of low-risk prostate cancers.
‘Magnetic resonance imaging (MRI) -based screening combined with blood tests would reduce prostate cancer-related deaths by 7–9 percent over a lifetime.’





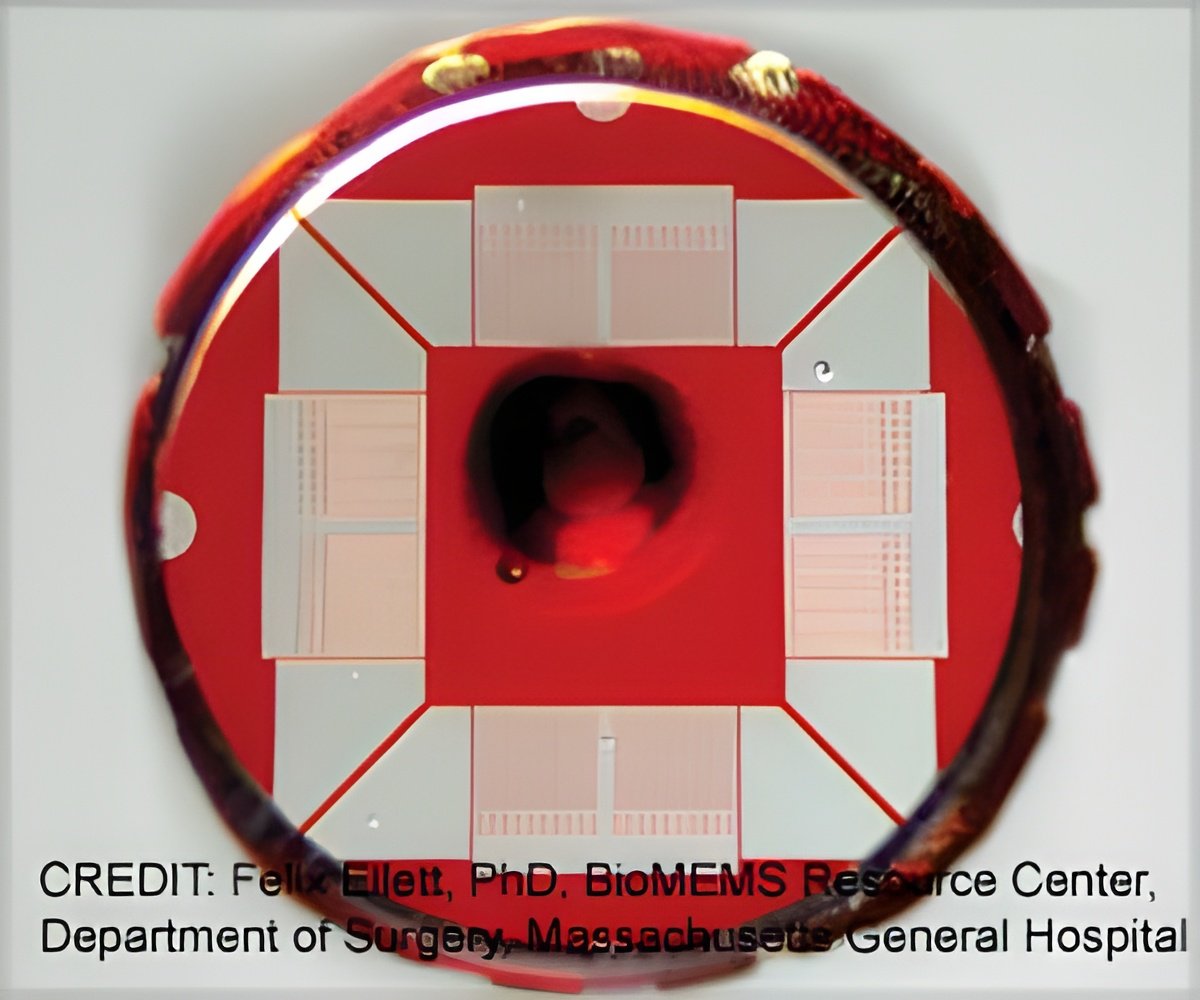
The clinical trial has previously shown that a blood test called Stockholm3, developed by researchers at Karolinska Institutet, can reduce the number of MRIs by a third for a single screening occasion.Now, the same research group reports that this combination is also considered cost-effective in Sweden compared with both no screening and PSA test in MRI-based screening.
“Our latest results show that using Stockholm3 reduces the number of MRIs over a lifetime by 60 percent. This also avoids unnecessary biopsies by 9 percent, which reduces the overdiagnosis of low-risk cancers,” says Mark Clements, associate professor at the Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, who is responsible for the cost-effectiveness study.
The health economic evaluation also showed that compared with no screening, screening with PSA followed by Stockholm3 and MRI in high-risk individuals is classified as a moderate cost per quality-adjusted life-years (QALY) gained as defined by the Swedish National Board of Health and Welfare.
Furthermore, PSA combined with MRI is classified as a very high cost per QALY gained compared with Stockholm3 combined with MRI.
Advertisement
The current health economic evaluation is specific to Sweden, but the simulation model used in this study is open source and can be readily adapted to assess the use of Stockholm3 and MRI in other countries.
Source-Medindia

![Prostate Specific Antigen [PSA] & Prostate Cancer Diagnosis Prostate Specific Antigen [PSA] & Prostate Cancer Diagnosis](https://images.medindia.net/patientinfo/120_100/prostate-specific-antigen.jpg)