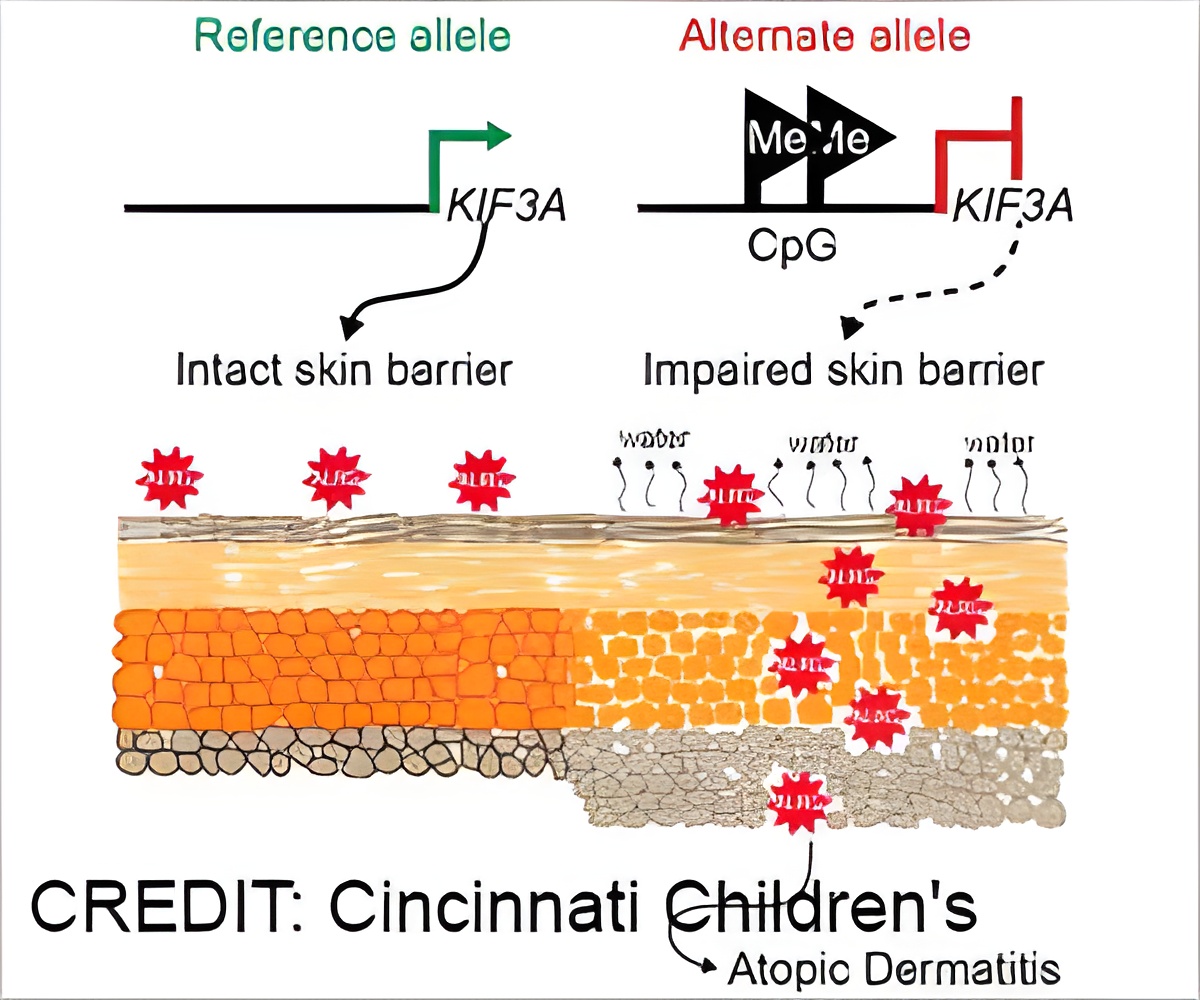
New variants in the KIF3A gene were found to help explain the link between skin disorder and food allergy risk.
‘New study findings could make it easier to identify which children with eczema are most likely to progress to other allergic conditions.’





These findings, led by scientists at Cincinnati Children's, were published online in Nature Communications. The first author was Mariana Stevens, PhD, and the senior corresponding author was Gurjit Khurana Hershey, MD, PhD, Director, Division of Asthma Research. The study sheds new light on the genetic and molecular mechanisms at work in atopic dermatitis, a common condition (also known as eczema) that affects as many as 20 percent of all children. Although eczema usually resolves as children age, many children with disrupted skin barriers go on to develop more severe conditions including asthma and food allergies.
This would allow lifestyle interventions and other preventive therapies to be targeted toward high-risk children. The study also suggests a new target for potential treatment.
"Food allergies are rising and the causes are not entirely clear," Hershey says. "This study adds evidence to a rising theory that skin health is more closely connected to lung and gut health than many have suspected."
Two tiny SNPs play big roles in skin health
Advertisement
Advertisement
Proper function of the KIF3A gene is important because it helps cells form their primary cilia, a structure on cell surfaces that acts as an antenna to receive important signal information from other cells. Previous studies led by experts at Cincinnati Children's and others have already shown that malfunctioning KIF3A in lung tissue can lead to asthma. Likewise, malfunctions of the same gene in gut tissues can increase risk of food allergies.
Now, this study helps connect both of these allergy risks to a damaged skin barrier, which allows more allergy-triggering substances to get inside our bodies to prompt immune system over-reactions.
"We are working to better understand how skin, gut and lung health are connected. In fact, we have a grant from the National Institutes of Health to further study this connection," Hershey says.
Development underway for screening test
The research team at Cincinnati Children's has begun searching for drug compounds that might someday be useful in restoring the disrupted functions of the KIF3A gene. But the first next step based on this study will be to continue an ongoing hunt for a rapid screening test.
The new study in Nature Communications builds on findings from two other studies published earlier this year from Cincinnati Children's scientists.
In February, a study in the Journal of Allergy and Clinical Immunology reported that the allergy risk posed by atopic dermatitis was higher than having a parent with allergic disease.
Then in April, a study in the same journal demonstrated the value of using pain-free tape stripping as a less-invasive tool than skin biopsies for gathering data about skin health.
The goal, Hershey says, would be to use skin tape strip samples to quantify KIF3A expression as a possible tool for predicting disease risk. The team is studying this approach in a group of 600 children from the Cincinnati region who were identified with atopic dermatitis early in life. This group, the first cohort of its kind in the US, will be followed for five years to directly evaluate the ability of KIF3A genetic variations and skin expression to predict disease risk.
Source-Eurekalert