New studies finds the link between the new genetic mutation and the hypothyroidism syndrome.
"ICSF1 involvement in central hypothyroidism is an important discovery because it creates inroads into our understanding of this rare syndrome, as well as new avenues by which it might be possible one day to control thyroid and testicular function," said Douglas Forrest, PhD, of the National Institute of Diabetes and Digestive and Kidney Diseases, and Program Co-Chair of the ATA Annual Meeting.
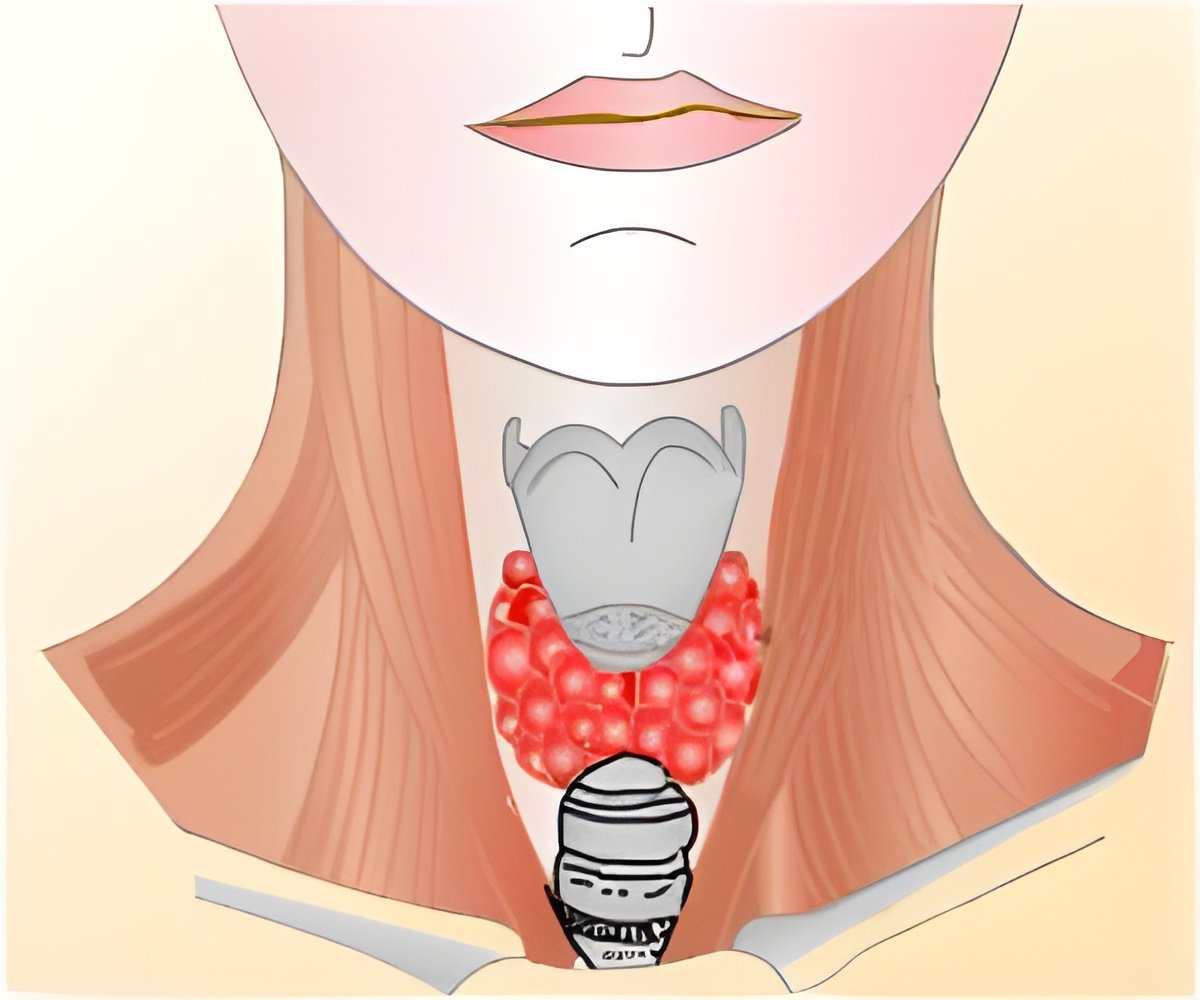
Central hypothyroidism is defined as hypothyroidism--a state in which the thyroid gland does not make enough thyroid hormone--due to insufficient stimulation by thyroid stimulating hormone (TSH) of an otherwise normal thyroid gland or in in conjunction with other pituitary hormone deficits. Undetected central hypothyroidism is associated with developmental delay in children and adverse cardiometabolic sequelae in adults. Until now, mutations in the thyrotropin-releasing hormone receptor (TRHR) or TSHb subunit (TSHB) genes had been the only known causes of isolated TSH deficiency.
A team of researchers led by Nadia Schoenmakers, PhD, at the University of Cambridge in the United Kingdom, studied 10 unrelated families with males exhibiting isolated TSH deficiency, testicular enlargement, and variably low serum prolactin levels. Using whole-exome and candidate gene sequencing, they identified nine distinct mutations in the X-linked immunoglobulin superfamily member 1 (IGSF1) gene in affected males. Their analyses revealed that IGSF1 encodes a pituitary-enriched plasma membrane glycoprotein and that disease-associated mutations block trafficking of IGSF1 from the endoplasmic reticulum to the membrane, consistent with the loss-of-protein function. In addition, the researchers characterized IGSF1-deficient mice and found that adult male IGSF1 null mice have decreased pituitary TSH content and circulating T4 levels and increased body weight and fat mass-characteristics that mimic features of the human disorder. Decreased TRHR mRNA levels in pituitaries from null mice, together with reduced TSH bioactivity in patients with IGSF1 mutations, suggest that impaired TRH signaling may be the basis for the disorder.
About the ATA Annual Meeting 

The 82nd Annual Meeting of the American Thyroid Association is held Sept. 19-23, in Québec City, Québec, Canada. This four-day creative and innovative scientific program, chaired by Elizabeth Pearce, MD, Boston Medical Center, and Douglas Forrest, PhD, National Institute of Diabetes and Digestive and Kidney Diseases, carefully balances clinical and basic science sessions on the latest advances in thyroidology. The ATA meeting is designed to offer continuing education for endocrinologists, internists, surgeons, basic scientists, nuclear medicine scientists, pathologists, endocrine fellows and nurses, physician assistants and other health care professionals.
Source-Newswise













